Ketogenic Diets for Cancer
The Ketogenic Diet may help with the treatment of cancer, including brain tumors[1][2][3]. Most of the available information comes from animal experiments, backed up with a few human case studies, but things look promising and human trials are occurring. There are even researchers who believe that the origin of cancer lies with metabolic abnormalities that lead to genetic problems rather than the genetic problems being the root cause[4]. Note that while the Ketogenic Diet may help with a number of diseases, the Ketogenic Diet also has some health risks. There are no indications that the Ketogenic Diet is a viable alternative to existing, traditional treatments, but it may become an important way of improving the success of the current approaches.
Contents
[hide]1 How the Ketogenic Diet may help
There may be several mechanisms behind the effect of the ketogenic diet on cancer. Some may also apply to a lesser extent to other Low Carbohydrate Diets, but some require Ketones. It seems reasonable that the benefits of the ketogenic diet for cancer patients rely on multiple underlying mechanisms.
- The ketogenic diet typically reduces blood glucose levels, and high blood glucose is associated with tumor growth and reduced survival rates in cancer patients[5][6][7] and animal models[8].
- Carbohydrate restriction lowers insulin and insulin-like growth factor (IGF) which directly stimulate tumor cell proliferation[9].
- Tumor cells are unable to metabolize ketones[10].
- Cancers promote the growth of new blood vessels, something the ketogenic diet inhibits, as Ketones are anti-angiogenic[11]. This is also seen with calorie restriction, which reduces vascularity and increased apoptosis in mouse and human brain tumors[12].
- Cancer cells often don't undergo natural cell death, something the ketogenic diet enhances[13].
- Ketones may directly reduce the viability of cancer cells[13].
2 Animal Studies
There are a number of animal studies that have looked at the ketogenic diet and cancer. Some of these studies combine the ketogenic diet with calorie restriction, while others provide an unrestricted access to food, and some are simply based around complete fasting. Obviously animal studies do not necessarily apply well to humans, but the evidence is encouraging.
- The ketogenic diet may need to be combined with calorie restriction to ensure lowered glucose levels for the treatment of brain tumors[14]. A study that compared an unrestricted standard diet, an unrestricted ketogenic diet and a restricted ketogenic diet in mice with implanted brain tumors, only the restricted ketogenic diet improved survival rates[11].
- The unrestricted ketogenic diet combined with Omega 3 and MCT delayed the growth of implanted gastric cancer cells in mice[15].
- Short term fasting can improve the survival rates for mice with implanted brain tumors, and this benefit can enhance both chemotherapy and radiation treatment[16].
- Drugs are being developed for cancer treatment that target metabolic pathways[17].
- Giving a no-carbohydrate ketogenic diet to rats with grafted prostate cancer tumors resulted in a 33% smaller tumor size than controls fed a western diet[18]. In another study, rats with grafted prostate cancer tumors given 0%, 10% or 20% carbohydrate had similar survival rates[19].
- Rats with grafted prostate cancer tumors given a no-carbohydrate ketogenic diet (83% fat, 0% carbohydrate, 17% protein) had a better survival rate than those given a medium carbohydrate diet (40% fat, 43% carbohydrate, 17% protein), but their survival was similar to those given a low fat diet (12% fat, 71% carbohydrate, 17% protein)[20].
- Rats with grafted lung cancer tumors showed that a ketogenic diet improved the effectiveness of radiation and chemotherapy[21].
- A study of Glioma tumor cells showed that an unrestricted ketogenic diet in mice that raised ketone levels without lowering glucose levels did not change survival rates[10].
- Rats with metastatic cancer had a 57% longer average survival time on the ketogenic diet than controls, and 78% longer when the ketogenic diet was combined with a hyperbaric oxygen therapy[22].
3 Human Case Studies
While I have not found any large studies of the ketogenic diet on humans, there are a number of smaller case studies that look promising.
- A case study of two children with inoperable Astrocytoma brain tumors that regressed under the ketogenic diet that lowered blood glucose levels is promising[23]. This trial used the MCT Diet with 60% of calories from MCT, 20% from protein, 10% from carbohydrate, and 10% from other dietary fats, with total calories calculated at 120% of target to ensure weight gain[24].
- A study looked at the use of the Ketogenic Diet in 16 patients with advanced cancer and no other treatment options concluded that the diet was a suitable possibility and might improve some aspects of their quality of life[25]. Not all the patients maintained the diet, with only 5 completing the 12 week study. Because of the low number of subjects and their heterogeneity, it was not possible to evaluate the impact of the diet on the tumors. However, the outcome for the 16 patients is intriguing:
- 4 patients dropped out early.
- 2 patients died early.
- 5 patients discontinued the diet and their disease progressed.
- 5 patients followed the diet and their disease was stable.
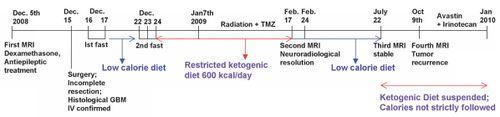
- A 65 year old woman with Glioblastoma multiforme (the most malignant primary brain tumor in adults and children) was treated with partial tumor resection and a combination of standard therapy and a restricted ketogenic diet. The diet was a calorie restricted (600 kcal/day) Ketogenic Ratio Diet (4:1) for two months, resulting in a 20% reduction in body weight. After the two months there were no discernable signs of the tumor with FDG-PET or MRI imaging[26]. When a normal diet was resumed for 10 weeks there were signs of the tumor resurging on MRI scans. (See timeline of treatment below.)
- A (non-ketogenic) high fat diet may help maintain body weight and improve quality of life[27].
4 Non-Ketogenic Fat Intake and Cancer
There are a number of studies that have looked at the general relationship between fat intake and cancer. Omega 3 may help inhibit cancer, while Omega 6, and to a lesser extent saturated fats, may exacerbate cancer.
- Fat intake in a non-ketogenic diet impacts tumor growth[28].
- Omega 3 supplementation may improve the effectiveness of conventional chemotherapy and radiation therapy treatments of cancer[29][30][31][32], as well as directly impacting the tumor[33][34][35][36][37] and metastasis[36][37].
- Omega-6 oils may increase tumor growth[36][38][28].
- Saturated fat tends to stimulate tumor growth, Omega-6 stimulates more than saturated fat, and Omega-3 inhibits growth[28].
- Omega-3 supplementation may reduce the risk of some cancers[40][41][42].
- In a study of 35,298 Singapore Chinese women aged 45-74 years, those with the lowest intake of fish Omega-3 had a 26% higher risk of breast cancer[43]. For those with the lowest intake of Omega-3, the intake of Omega-6 was inversely related to their breast cancer risk. However, another study of 23,693 postmenopausal women showed that fish consumption increased the risk of estrogen receptor-positive breast cancer by 50% in those with the highest intake compared with the lowest[44]. It has been suggested that this may be due to contamination with organochlorines or other endocrine disrupters in the fish[45]. Other studies have found no relationship between fish intake and cancer[46][47].
- The results of trials with mono-unsaturated oils such as olive oils on tumor growth have been inconsistent[28].
- Restricting calories intake also impacts tumor growth, with 12% restriction reducing tumor growth in rodents[28].
- Even modest amounts of Omega-6 or saturated fat may negate the benefit of Omega-3[28].
5 Further Reading
In addition to the scientific papers referenced in this article, there are some books that may be useful.
5.1 Ketogenic Diets: Treatments for Epilepsy and Other Disorders
Ketogenic Diets: Treatments for Epilepsy and Other Disorders, by Eric H. Kossoff is the best all-around book I've come across on the ketogenic diet, and while it focuses heavily on epilepsy, it does touch on other conditions. If you are considering the Ketogenic Diet, I would consider this as essential reading. It has a positive view of the ketogenic diet, but balances this with the caution that comes with being a medical practitioner that has used the diet for many years.
5.2 Anticancer
Anticancer is a book by David Servan-Schreiber. In the book, David describes his personal battle with brain cancer, and the research he did to understand why we get cancer. The book presents a grim warning of the cancer epidemic that is occurring in the western world, with age-adjusted cancer rates steadily rising since the 1940s. However, the book also offers hope, as there are useful that may help fight cancer. Anticancer is an approach that may reduce our risk of getting cancer, and for those with the disease, it might supplement surgery, chemotherapy and radiation as treatments. The book claims that genes only comprise 15% of the risk for cancer, with smoking and diet contributing 30% each. There are several parts to the anticancer approach:
- The book suggests that the immune system forms a defense against cancer. If our immune system is compromised, then cancer can grow.
- Avoid high Glycemic Index foods. Having continuously elevated blood sugar and insulin levels causes chronic inflammation that compromises the immune system and provides growth hormones the fuel cancerous growth. High Glycemic Index foods are also linked to obesity, diabetes, and heart disease.
- Eat foods with anticancer properties, such as curry, green tea, soy, garlic. The book contains a longer list, and there is another book Foods to Fight Cancer with more information. I have not looked at the research that supports these foods.
- Boost Omega 3 intake and reduce Omega 6 intake, aiming for a 1:1 ratio of Omega-3 to Omega-6. This ratio is found in grass fed animal products, or it can be achieved through foods rich in Omega-3 such as fatty fish or Flax. All Trans Fats should be avoided (look for "partially hydrogenated" in the ingredients to identify trans fats).
- Detoxify by not consuming poisons. This primarily means eating more organic food, especially animal products such as meat or dairy. For non-animal products, some are worth getting organic, whereas others pose a more limited risk. There is a list of the 12 least contaminated and 12 most contaminated foods at The Dirty Dozen.
- Exercise for at least 20 to 30 minutes per day. The book notes that different types of cancers require different levels of exercise to achieve a comparable effect; for instance, colon cancer requires twice as much as breast cancer.
- Feelings of helplessness ( External Locus of Control) and past emotional traumas compromise our body's ability to fight cancer. For some, exercise can restore our feeling of control over our lives, but counseling may also be needed.
- Meditation, including Yoga, tai chi, etc., helps reduce stress.
5.3 Cancer as a Metabolic Disease
This book, "Cancer as a Metabolic Disease: On the Origin, Management, and Prevention of Cancer" by Dr. Thomas Seyfried, is an expensive, technical book by one of the leading researchers in this field. It's recommended if you want to research more deeply into this topic. There is also a smaller and cheaper eBook called "Fight Cancer with a Ketogenic Diet" that is based on Seyfried's book.
6 See Also
- The classifications and types of Low Carbohydrate Diet.
- An introduction to the Ketogenic Diet.
- My experiences with ultrarunning on the Ketogenic Diet
- How the Ketogenic Diet can be used for the treatment and management of disease.
- Using the Ketogenic Diets to mitigate and treat Epilepsy
- How Ketogenic Diets might help with Cancer
- A look at the possible mechanisms of action of the Ketogenic Diet
- Health Risks of the Ketogenic Diet
- The time frame and changes that occur with Ketoadaptation
- What are Ketones
- The pros and cons of the Ketogenic Diet for athletes
- The Types of Ketogenic Diet
- How the Ketogenic Diet can be used for the treatment and management of disease.
- My Ketogenic Recipes
- Non-Ketogenic Low Carbohydrate Diets
7 References
- Jump up ↑ TN. Seyfried, MA. Kiebish, J. Marsh, LM. Shelton, LC. Huysentruyt, P. Mukherjee, Metabolic management of brain cancer., Biochim Biophys Acta, volume 1807, issue 6, pages 577-94, Jun 2011, doi 10.1016/j.bbabio.2010.08.009, PMID 20804725
- Jump up ↑ BT. Seyfried, M. Kiebish, J. Marsh, P. Mukherjee, Targeting energy metabolism in brain cancer through calorie restriction and the ketogenic diet., J Cancer Res Ther, volume 5 Suppl 1, pages S7-15, Sep 2009, doi 10.4103/0973-1482.55134, PMID 20009300
- Jump up ↑ TN. Seyfried, P. Mukherjee, Targeting energy metabolism in brain cancer: review and hypothesis., Nutr Metab (Lond), volume 2, pages 30, Oct 2005, doi 10.1186/1743-7075-2-30, PMID 16242042
- Jump up ↑ T. N. Seyfried, R. Flores, A. M. Poff, D. P. D'Agostino, Cancer as a Metabolic Disease: Implications for Novel Therapeutics, Carcinogenesis, 2013, ISSN 0143-3334, doi 10.1093/carcin/bgt480
- Jump up ↑ KL. Chaichana, MJ. McGirt, GF. Woodworth, G. Datoo, RJ. Tamargo, J. Weingart, A. Olivi, H. Brem, A. Quinones-Hinojosa, Persistent outpatient hyperglycemia is independently associated with survival, recurrence and malignant degeneration following surgery for hemispheric low grade gliomas., Neurol Res, volume 32, issue 4, pages 442-8, May 2010, doi 10.1179/174313209X431101, PMID 19589201
- Jump up ↑ RL. Derr, X. Ye, MU. Islas, S. Desideri, CD. Saudek, SA. Grossman, Association between hyperglycemia and survival in patients with newly diagnosed glioblastoma., J Clin Oncol, volume 27, issue 7, pages 1082-6, Mar 2009, doi 10.1200/JCO.2008.19.1098, PMID 19139429
- Jump up ↑ MJ. McGirt, KL. Chaichana, M. Gathinji, F. Attenello, K. Than, AJ. Ruiz, A. Olivi, A. Quiñones-Hinojosa, Persistent outpatient hyperglycemia is independently associated with decreased survival after primary resection of malignant brain astrocytomas., Neurosurgery, volume 63, issue 2, pages 286-91; discussion 291, Aug 2008, doi 10.1227/01.NEU.0000315282.61035.48, PMID 18797358
- Jump up ↑ V. Venkateswaran, AQ. Haddad, NE. Fleshner, R. Fan, LM. Sugar, R. Nam, LH. Klotz, M. Pollak, Association of diet-induced hyperinsulinemia with accelerated growth of prostate cancer (LNCaP) xenografts., J Natl Cancer Inst, volume 99, issue 23, pages 1793-800, Dec 2007, doi 10.1093/jnci/djm231, PMID 18042933
- Jump up ↑ RJ. Klement, U. Kämmerer, Is there a role for carbohydrate restriction in the treatment and prevention of cancer?, Nutr Metab (Lond), volume 8, pages 75, 2011, doi 10.1186/1743-7075-8-75, PMID 22029671
- ↑ Jump up to: 10.0 10.1 GD. Maurer, DP. Brucker, O. Bähr, PN. Harter, E. Hattingen, S. Walenta, W. Mueller-Klieser, JP. Steinbach, J. Rieger, Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for ketogenic diet as experimental glioma therapy., BMC Cancer, volume 11, pages 315, 2011, doi 10.1186/1471-2407-11-315, PMID 21791085
- ↑ Jump up to: 11.0 11.1 W. Zhou, P. Mukherjee, MA. Kiebish, WT. Markis, JG. Mantis, TN. Seyfried, The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer., Nutr Metab (Lond), volume 4, pages 5, 2007, doi 10.1186/1743-7075-4-5, PMID 17313687
- Jump up ↑ P. Mukherjee, LE. Abate, TN. Seyfried, Antiangiogenic and proapoptotic effects of dietary restriction on experimental mouse and human brain tumors., Clin Cancer Res, volume 10, issue 16, pages 5622-9, Aug 2004, doi 10.1158/1078-0432.CCR-04-0308, PMID 15328205
- ↑ Jump up to: 13.0 13.1 R. Skinner, A. Trujillo, X. Ma, EA. Beierle, Ketone bodies inhibit the viability of human neuroblastoma cells., J Pediatr Surg, volume 44, issue 1, pages 212-6; discussion 216, Jan 2009, doi 10.1016/j.jpedsurg.2008.10.042, PMID 19159745
- Jump up ↑ TN. Seyfried, M. Kiebish, P. Mukherjee, J. Marsh, Targeting energy metabolism in brain cancer with calorically restricted ketogenic diets., Epilepsia, volume 49 Suppl 8, pages 114-6, Nov 2008, doi 10.1111/j.1528-1167.2008.01853.x, PMID 19049606
- Jump up ↑ C. Otto, U. Kaemmerer, B. Illert, B. Muehling, N. Pfetzer, R. Wittig, HU. Voelker, A. Thiede, JF. Coy, Growth of human gastric cancer cells in nude mice is delayed by a ketogenic diet supplemented with omega-3 fatty acids and medium-chain triglycerides., BMC Cancer, volume 8, pages 122, 2008, doi 10.1186/1471-2407-8-122, PMID 18447912
- Jump up ↑ F. Safdie, S. Brandhorst, M. Wei, W. Wang, C. Lee, S. Hwang, PS. Conti, TC. Chen, VD. Longo, Fasting enhances the response of glioma to chemo- and radiotherapy., PLoS One, volume 7, issue 9, pages e44603, 2012, doi 10.1371/journal.pone.0044603, PMID 22984531
- Jump up ↑ DA. Tennant, RV. Durán, E. Gottlieb, Targeting metabolic transformation for cancer therapy., Nat Rev Cancer, volume 10, issue 4, pages 267-77, Apr 2010, doi 10.1038/nrc2817, PMID 20300106
- Jump up ↑ SJ. Freedland, J. Mavropoulos, A. Wang, M. Darshan, W. Demark-Wahnefried, WJ. Aronson, P. Cohen, D. Hwang, B. Peterson, Carbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axis., Prostate, volume 68, issue 1, pages 11-9, Jan 2008, doi 10.1002/pros.20683, PMID 17999389
- Jump up ↑ EM. Masko, JA. Thomas, JA. Antonelli, JC. Lloyd, TE. Phillips, SH. Poulton, MW. Dewhirst, SV. Pizzo, SJ. Freedland, Low-carbohydrate diets and prostate cancer: how low is "low enough"?, Cancer Prev Res (Phila), volume 3, issue 9, pages 1124-31, Sep 2010, doi 10.1158/1940-6207.CAPR-10-0071, PMID 20716631
- Jump up ↑ JC. Mavropoulos, WC. Buschemeyer, AK. Tewari, D. Rokhfeld, M. Pollak, Y. Zhao, PG. Febbo, P. Cohen, D. Hwang, The effects of varying dietary carbohydrate and fat content on survival in a murine LNCaP prostate cancer xenograft model., Cancer Prev Res (Phila), volume 2, issue 6, pages 557-65, Jun 2009, doi 10.1158/1940-6207.CAPR-08-0188, PMID 19470786
- Jump up ↑ B. G. Allen, S. K. Bhatia, J. M. Buatti, K. E. Brandt, K. E. Lindholm, A. M. Button, L. I. Szweda, B. J. Smith, D. R. Spitz, M. A. Fath, Ketogenic Diets Enhance Oxidative Stress and Radio-Chemo-Therapy Responses in Lung Cancer Xenografts, Clinical Cancer Research, volume 19, issue 14, 2013, pages 3905–3913, ISSN 1078-0432, doi 10.1158/1078-0432.CCR-12-0287
- Jump up ↑ Chih-Hsin Tang, Angela M. Poff, Csilla Ari, Thomas N. Seyfried, Dominic P. D'Agostino, The Ketogenic Diet and Hyperbaric Oxygen Therapy Prolong Survival in Mice with Systemic Metastatic Cancer, PLoS ONE, volume 8, issue 6, 2013, pages e65522, ISSN 1932-6203, doi 10.1371/journal.pone.0065522
- Jump up ↑ LC. Nebeling, F. Miraldi, SB. Shurin, E. Lerner, Effects of a ketogenic diet on tumor metabolism and nutritional status in pediatric oncology patients: two case reports., J Am Coll Nutr, volume 14, issue 2, pages 202-8, Apr 1995, PMID 7790697
- Jump up ↑ LC. Nebeling, E. Lerner, Implementing a ketogenic diet based on medium-chain triglyceride oil in pediatric patients with cancer., J Am Diet Assoc, volume 95, issue 6, pages 693-7, Jun 1995, doi 10.1016/S0002-8223(95)00189-1, PMID 7759747
- Jump up ↑ Melanie Schmidt, Nadja Pfetzer, Micheal Schwab, Ingrid Strauss, Ulrike Kämmerer, Effects of a ketogenic diet on the quality of life in 16 patients with advanced cancer: A pilot trial, Nutrition & Metabolism, volume 8, issue 1, 2011, pages 54, ISSN 1743-7075, doi 10.1186/1743-7075-8-54
- Jump up ↑ Giulio Zuccoli, Norina Marcello, Anna Pisanello, Franco Servadei, Salvatore Vaccaro, Purna Mukherjee, Thomas N Seyfried, Metabolic management of glioblastoma multiforme using standard therapy together with a restricted ketogenic diet: Case Report, Nutrition & Metabolism, volume 7, issue 1, 2010, pages 33, ISSN 1743-7075, doi 10.1186/1743-7075-7-33
- Jump up ↑ R. Breitkreutz, K. Tesdal, D. Jentschura, O. Haas, H. Leweling, E. Holm, Effects of a high-fat diet on body composition in cancer patients receiving chemotherapy: a randomized controlled study., Wien Klin Wochenschr, volume 117, issue 19-20, pages 685-92, Oct 2005, doi 10.1007/s00508-005-0455-3, PMID 16416368
- ↑ Jump up to: 28.0 28.1 28.2 28.3 28.4 28.5 CW. Welsch, Dietary fat, calories, and mammary gland tumorigenesis., Adv Exp Med Biol, volume 322, pages 203-22, 1992, PMID 1442296
- Jump up ↑ WE. Hardman, (n-3) fatty acids and cancer therapy., J Nutr, volume 134, issue 12 Suppl, pages 3427S-3430S, Dec 2004, PMID 15570049
- Jump up ↑ WE. Hardman, Omega-3 fatty acids to augment cancer therapy., J Nutr, volume 132, issue 11 Suppl, pages 3508S-3512S, Nov 2002, PMID 12421878
- Jump up ↑ H. Xue, S. Le Roy, MB. Sawyer, CJ. Field, LA. Dieleman, VE. Baracos, Single and combined supplementation of glutamine and n-3 polyunsaturated fatty acids on host tolerance and tumour response to 7-ethyl-10-[4-(1-piperidino)-1-piperidino]carbonyloxy-camptothecin (CPT-11)/5-fluorouracil chemotherapy in rats bearing Ward colon tumour., Br J Nutr, volume 102, issue 3, pages 434-42, Aug 2009, doi 10.1017/S0007114508199482, PMID 19250573
- Jump up ↑ YM. Dupertuis, MM. Meguid, C. Pichard, Colon cancer therapy: new perspectives of nutritional manipulations using polyunsaturated fatty acids., Curr Opin Clin Nutr Metab Care, volume 10, issue 4, pages 427-32, Jul 2007, doi 10.1097/MCO.0b013e3281e2c9d4, PMID 17563460
- Jump up ↑ CN. Gutt, L. Brinkmann, A. Mehrabi, H. Fonouni, BP. Müller-Stich, G. Vetter, JM. Stein, P. Schemmer, MW. Büchler, Dietary omega-3-polyunsaturated fatty acids prevent the development of metastases of colon carcinoma in rat liver., Eur J Nutr, volume 46, issue 5, pages 279-85, Aug 2007, doi 10.1007/s00394-007-0662-y, PMID 17593466
- Jump up ↑ WE. Hardman, Dietary canola oil suppressed growth of implanted MDA-MB 231 human breast tumors in nude mice., Nutr Cancer, volume 57, issue 2, pages 177-83, 2007, doi 10.1080/01635580701277445, PMID 17571951
- Jump up ↑ T. Kato, RL. Hancock, H. Mohammadpour, B. McGregor, P. Manalo, S. Khaiboullina, MR. Hall, L. Pardini, RS. Pardini, Influence of omega-3 fatty acids on the growth of human colon carcinoma in nude mice., Cancer Lett, volume 187, issue 1-2, pages 169-77, Dec 2002, PMID 12359365
- ↑ Jump up to: 36.0 36.1 36.2 DP. Rose, JM. Connolly, J. Rayburn, M. Coleman, Influence of diets containing eicosapentaenoic or docosahexaenoic acid on growth and metastasis of breast cancer cells in nude mice., J Natl Cancer Inst, volume 87, issue 8, pages 587-92, Apr 1995, PMID 7752256
- ↑ Jump up to: 37.0 37.1 DP. Rose, JM. Connolly, M. Coleman, Effect of omega-3 fatty acids on the progression of metastases after the surgical excision of human breast cancer cell solid tumors growing in nude mice., Clin Cancer Res, volume 2, issue 10, pages 1751-6, Oct 1996, PMID 9816126
- Jump up ↑ DP. Rose, JM. Connolly, CL. Meschter, Effect of dietary fat on human breast cancer growth and lung metastasis in nude mice., J Natl Cancer Inst, volume 83, issue 20, pages 1491-5, Oct 1991, PMID 1920496
- Jump up ↑ SD. Hursting, M. Thornquist, MM. Henderson, Types of dietary fat and the incidence of cancer at five sites., Prev Med, volume 19, issue 3, pages 242-53, May 1990, PMID 2377587
- Jump up ↑ RA. Karmali, n-3 fatty acids and cancer., J Intern Med Suppl, volume 731, pages 197-200, 1989, PMID 2539832
- Jump up ↑ PD. Terry, TE. Rohan, A. Wolk, Intakes of fish and marine fatty acids and the risks of cancers of the breast and prostate and of other hormone-related cancers: a review of the epidemiologic evidence., Am J Clin Nutr, volume 77, issue 3, pages 532-43, Mar 2003, PMID 12600840
- Jump up ↑ EA. de Deckere, Possible beneficial effect of fish and fish n-3 polyunsaturated fatty acids in breast and colorectal cancer., Eur J Cancer Prev, volume 8, issue 3, pages 213-21, Jul 1999, PMID 10443950
- Jump up ↑ M. Gago-Dominguez, JM. Yuan, CL. Sun, HP. Lee, MC. Yu, Opposing effects of dietary n-3 and n-6 fatty acids on mammary carcinogenesis: The Singapore Chinese Health Study., Br J Cancer, volume 89, issue 9, pages 1686-92, Nov 2003, doi 10.1038/sj.bjc.6601340, PMID 14583770
- Jump up ↑ C. Stripp, K. Overvad, J. Christensen, BL. Thomsen, A. Olsen, S. Møller, A. Tjønneland, Fish intake is positively associated with breast cancer incidence rate., J Nutr, volume 133, issue 11, pages 3664-9, Nov 2003, PMID 14608091
- Jump up ↑ PD. Terry, JB. Terry, TE. Rohan, Long-chain (n-3) fatty acid intake and risk of cancers of the breast and the prostate: recent epidemiological studies, biological mechanisms, and directions for future research., J Nutr, volume 134, issue 12 Suppl, pages 3412S-3420S, Dec 2004, PMID 15570047
- Jump up ↑ MD. Holmes, GA. Colditz, DJ. Hunter, SE. Hankinson, B. Rosner, FE. Speizer, WC. Willett, Meat, fish and egg intake and risk of breast cancer., Int J Cancer, volume 104, issue 2, pages 221-7, Mar 2003, doi 10.1002/ijc.10910, PMID 12569578
- Jump up ↑ S. A Missmer, Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies, International Journal of Epidemiology, volume 31, issue 1, 2002, pages 78–85, ISSN 14643685, doi 10.1093/ije/31.1.78