Difference between revisions of "NSAIDs and Running"
User:Fellrnr (User talk:Fellrnr | contribs) m (→NSAIDs and Intestinal Damage) |
User:Fellrnr (User talk:Fellrnr | contribs) |
||
| (16 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| − | {{DISPLAYTITLE: NSAIDs (Ibuprofen, Acetaminophen/Paracetamol | + | {{DISPLAYTITLE: NSAIDs (Ibuprofen, Naproxen, Aspirin) and Acetaminophen/Paracetamol for runners, impairs healing and interferes with hydration}} |
[[File:Extra Strength Tylenol and Tylenol PM.jpg|right|thumb|200px|Acetaminophen (brand names Tylenol, aspirin-free Anacin, Excedrin, and numerous cold medicines)]] | [[File:Extra Strength Tylenol and Tylenol PM.jpg|right|thumb|200px|Acetaminophen (brand names Tylenol, aspirin-free Anacin, Excedrin, and numerous cold medicines)]] | ||
| − | NSAIDs are Non-Steroidal Anti-Inflammatory Drugs | + | NSAIDs are generally unhelpful for runners, masking the symptoms while impairing healing, interfering with hydration and can be life threatening. Risks include kidney failure, heart attacks, strokes, intestinal damage, and liver failure. The most common NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are Ibuprofen (Advil, Motrin), Naproxen (Aleve, Naprosyn), and Aspirin. They work by inhibiting a particular enzyme ([http://en.wikipedia.org/wiki/Cyclooxygenase Cyclooxygenase]) which reduces pain, fever and inflammation. Ibuprofen use is so common among runners that it is sometimes called "Vitamin I"<ref name="VitaminI"/>, with one study finding about 60% of runners using NSAIDs during training<ref name="JoslinLloyd2013"/>. This is unsurprising given the estimates of injury rates in runners varying between 20% and 80%<ref name="vanGent-2007"/>. This article also covers Acetaminophen (also called Paracetamol), though it's not technically an NSAID. |
| − | + | =NSAIDs and Healing= | |
The inflammation response of our bodies is a key part of the healing process. Using NSAIDs to reduce the inflammation has been shown to impair healing in different tissue types: | The inflammation response of our bodies is a key part of the healing process. Using NSAIDs to reduce the inflammation has been shown to impair healing in different tissue types: | ||
| − | * | + | * '''Muscles'''<ref name="MuscleTrappe"/>. A 2001 study showed that Ibuprofen and Acetaminophen reduce [[Muscle|muscle]] growth after eccentric exercise. Another study<ref name="muscle"/> on muscle damage and NSAIDs showed impaired recovery in the early stages of healing. There was some increased [[Protein]] synthesis with NSAIDs in latter stages of healing, but the muscles were still weaker 28 days after injury. Other studies<ref name="muscle2"/><ref name="muscle3"/> have shown that four days after injury, NSAIDs resulted in very little muscle regeneration compared with no drugs. |
| − | * | + | * '''Tendons'''. A primate study<ref name="TendonPrimates"/> showed "a marked decrease in the breaking strength of tendons at four and six weeks in the ibuprofen-treated animals". Another animal study<ref name="TendonCOX2"/> showed treated tendons were 32% weaker than their untested counterparts. A study of older adults showed a weakening of tendons with acetaminophen (but not ibuprofen) use<ref name="CarrollDickinson2011"/>. |
| − | * | + | * '''Bone-Tendon Junctions'''. An animal study<ref name="tendon"/> of rotator cuff injuries shows that NSAID usage resulted in injuries that did not heal, and those that did heal were weaker than those without NSAID. To quote from the study "Given that NSAID administration was discontinued after 14 days yet affected load-to-failure eight weeks following repair, it appears that inhibition of the early events in the inflammatory cascade has a lasting negative effect on tendon-to-bone healing," Dr. Rodeo said. |
| − | * | + | * '''Cartilage. ''' NSAIDs have been shown<ref name="CartilageRabbit"/> to impair the healing of bone and cartilage in rabbits. |
| − | * | + | * '''Bone fractures.''' Tests on rats shows that a NSAID (Celecoxib) in the early stages of bone healing impaired healing, producing a weaker repair.<ref name="bone"/> A study <ref name="BoneLaurence "/> in 2004 declared " Nonsteroidal anti-inflammatory drugs continue to be prescribed as analgesics for patients with healing fractures even though these drugs diminish bone formation, healing, and remodeling". |
| − | + | ==Counterpoint== | |
While there is extensive experimental evidence for NSAIDs impairing healing, there are also some studies that show no change with NSAID use, and a few that indicated improved healing. For instance, one study<ref name="LigamentImprovement"/> showed that using an NSAID for 6 days after injury resulted in a 42% increased ligament strength at day 14, though there was no change by day 21. Another study<ref name="LigamentUninjuredImprovement"/> showed that an NSAID did not change ligament healing, but did improve the strength of the uninjured ligaments. However, my reading indicates that the preponderance of evidence shows NSAIDs impair healing. | While there is extensive experimental evidence for NSAIDs impairing healing, there are also some studies that show no change with NSAID use, and a few that indicated improved healing. For instance, one study<ref name="LigamentImprovement"/> showed that using an NSAID for 6 days after injury resulted in a 42% increased ligament strength at day 14, though there was no change by day 21. Another study<ref name="LigamentUninjuredImprovement"/> showed that an NSAID did not change ligament healing, but did improve the strength of the uninjured ligaments. However, my reading indicates that the preponderance of evidence shows NSAIDs impair healing. | ||
| − | + | ==Ice, Inflammation and Healing== | |
| − | If NSAIDs are bad for healing, should we treat with ice? So far I have found no definitive studies, but ice has a | + | If NSAIDs are bad for healing, should we treat with ice? So far I have found no definitive studies, but ice has a different mechanism of action from NSAIDs. By cooling the tissues, ice temporarily reduces swelling, thereby flushing the wound. If applied for a longer period of time, ice will produce a periodic increase in blood supply that creates a further flushing effect. I have found that ice can produce dramatic improvements in healing speed. See [[Cryotherapy - Ice for Healing]] for more details. There is no evidence that ice reduces any of the inflammation processes. |
| − | + | =Turmeric as an NSAID= | |
| + | [[File:Curcuma longa roots.jpg|right|thumb|300px|Turmeric rhizome and powder (By Simon A. Eugster - Own work, CC BY-SA 3.0).]] | ||
| + | Turmeric is an anti-inflammatory<ref name="Sahebkar2014"/><ref name="PanahiSahebkar2012"/> that is often considered an alternative to more common NSAIDs. Like other NSAIDs, Turmeric is an effective pain reliever (analgesic)<ref name="Agarwal-2011"/><ref name="Panahi-2014"/><ref name="Kuptniratsaikul-2009"/><ref name="Zhu-2014"/> and it may be effective in treating [[Delayed Onset Muscle Soreness]]<ref name="Nicol-2015"/><ref name="Drobnic-2014"/><ref name="McFarlinVenable2016"/><ref name="TanabeMaeda2015"/><ref name="Davis-2007"/><ref name="Kawanishi-2013"/>. Studies of Turmeric and turmeric derivatives as treatments for osteoarthritis<ref name="Henrotin-2014"/><ref name="Kuptniratsaikul-2014"/>, rheumatoid arthritis<ref name="Chandran-2012"/>, and cancer<ref name="Cheng-2001"/><ref name="RaoDinkar2013"/><ref name="Gupta-2013"/> show potentially promising results. However, there are concerns that most of the human studies on Turmeric are of poor quality and should be treated with caution<ref name="Mancuso-2009"/>. | ||
| + | ==Turmeric Safety== | ||
| + | Turmeric has been medicinally used for 1000s of years<ref name="Benzie-"/> and even in large doses turmeric shows low acute toxicity<ref name="Hsu-2007"/><ref name="Cheng-2001"/><ref name="Chandran-2012"/><ref name="GanigerMalleshappa2007"/> with only a few studies finding nausea and diarrhea<ref name="Hsu-2007"/> or abdominal pain<ref name="Kuptniratsaikul-2014"/>. However, there are concerns that many studies on Turmeric are in vitro (isolated tissues) at dose levels that are hard to replicate in humans<ref name="Burgos-MorónCalderón-Montaño2010"/>. Doses as high as 12g of curcumin produce negligible levels in the blood<ref name="VareedKakarala2008"/>. At therapeutic levels there is evidence that Turmeric (curcumin) may be carcinogenic<ref name="GoodpastureArrighi1976"/><ref name="Giri-1990"/><ref name="Ahsan-1998"/><ref name="Sakano-2002"/><ref name="Nair-2005"/><ref name="Blasiak-1999"/><ref name="Kelly-2001"/><ref name="Cao-2006"/><ref name="Urbina-Cano-2006"/>, though it can exhibit both anticancer and carcinogenic properties<ref name="López-Lázaro-2008"/>. Curcumin can inhibit liver function, including the drug-metabolizing P450 enzymes<ref name="Hayeshi-2007"/><ref name="Basu-2004"/><ref name="Oetari-1996"/><ref name="Appiah-Opong-2007"/><ref name="Volak-2008"/>. (This could cause problematic drug interactions.) Turmeric may bind to iron, resulting in iron deficiency<ref name="Jiao-2009"/><ref name="Baum-2004"/>, though it has been suggested that some of the benefits of Turmeric are from this iron binding<ref name="Means2008"/>. It should be remembered that other common constituents of normal diet have shown to be toxic when used as dietary supplements<ref name="Goodman-2004"/> | ||
| + | ==Turmeric Doses== | ||
| + | It's been estimated people in India consuming high culinary intakes of Turmeric obtain about 150mg/day of curcumin<ref name="Sharma-2005"/>, and average intake is probably 60-100mg/day<ref name="Shah-1999"/>. However, must studies use much higher levels, and culinary levels (~2g/day) Turmeric is probably ineffective as an NSAID<ref name="NiemanCialdella-Kam2012"/>. Turmeric has poor bioavailability<ref name="Anand-2010"/><ref name="AnandKunnumakkara2007"/> due to poor absorption and rapid metabolism<ref name="AnandKunnumakkara2007"/>. The curcumin level in Turmeric powder can vary dramatically, with one study finding levels between 0.6 and 3.1% dry weight, a more than five-fold variation<ref name="TayyemHeath2006"/>. This makes it hard to use the raw powder, as the actual dose could vary enormously and a high dose of curcumin such as 8g would potentially require the consumption of 1.3Kg/2.8 pounds of Turmeric powder. It's been shown that 3.6 g curcumin produces effective levels in the digestive system, but negligible levels outside the gut<ref name="Garcea-2005"/>, and even 12g of curcumin produce negligible levels in the blood<ref name="VareedKakarala2008"/>. This is compounded by the rapid removal, with concentrations of curcumin typically peak 1-2 hours after consumption and declining within 12 hours<ref name="Cheng-2001"/><ref name="Agarwal-2011"/>. At this point, it's hard to define a dose of Turmeric or curcumin beyond saying that it's safe at culinary levels (~2g/day of Turmeric powder). | ||
| + | ==Turmeric Enhancers== | ||
| + | The levels of Turmeric can be enhanced by taking it with piperine, a constituent of black pepper. One study that gave subjects 2g of curcumin found extremely low levels in the blood, but adding 20mg of piperine boosted blood levels by 2000%<ref name="Shoba-1998"/>. Another animal study using intravenous administration found piperine enhanced the effectiveness of curcumin<ref name="BhutaniBishnoi2009"/>. However, an animal study found that low levels (20 mg/kg) of piperine did not enhance the effectiveness of curcumin, and higher levels (40 mg/kg) actually negated the curcumin benefits<ref name="Arcaro-2014"/>. Piperine increases the absorption of curcumin<ref name="Suresh-2010"/> and reduces the metabolism of curcumin by the liver<ref name="Shoba-1998"/><ref name="Volak-2008"/>. However, the reduced metabolism is because like curcumin, piperine is a powerful inhibitor of liver function<ref name="Atal-1985"/><ref name="Bhardwaj-2002"/><ref name="Singh-1986"/>. Personally, I am cautious about boosting the levels of curcumin by impairing the liver. There are also versions of curcumin with improved bioavailability are being developed such as Flexofytol<ref name="AppelboomMaes2014"/> or Meriva<ref name="Drobnic-2014"/>. However, it should be noted that the bulk of the current research does not use enhancers, so caution may be appropriate. | ||
| + | ==Turmeric as a selective COX-2 Inhibitor== | ||
| + | Digestive problems, a common side effect of NSAIDs, are believed to be because most NSAIDs inhibit both COX-1 and COX-2 enzymes<ref name="Bertolini-2002"/>. COX-2 is predominantly responsible for inflammation where COX-1 helps maintain the digestive system<ref name="Hawkey-2001"/>. Selectively inhibiting just COX-2 may have the benefits of NSAIDS without the digestive issues<ref name="FutakiTakahashi1994"/><ref name="Hawkey1999"/><ref name="Hawkey-2001"/>. Studies have found that Turmeric is a COX-2 inhibitor<ref name="Moini Zanjani-2014"/><ref name="Moriyuki-2010"/><ref name="Ireson-2001"/><ref name="Lev-Ari-2006"/><ref name="Plummer-1999"/>, and turmeric preferentially inhibits COX-2 over COX-1<ref name="RamsewakDeWitt2000"/>. Turmeric has ~36% COX-1 inhibition and ~77% COX-2 inhibition, while aspirin, ibuprofen and naproxen had 41-52% COX-1 inhibition and ~30-40% COX-2 inhibition<ref name="RamsewakDeWitt2000"/>. Diferuloylmethane (Curcumin) is the main active ingredient in turmeric<ref name="Anand-2010"/><ref name="Henrotin-2010"/>, though it also includes monodemethoxycurcumin (curcumin II) and bisdemethoxycurcumin (curcumin III)<ref name="RamsewakDeWitt2000"/>. | ||
=NSAIDs and Acute kidney failure= | =NSAIDs and Acute kidney failure= | ||
| − | Kidney failure while running is extremely rare, and seems to require multiple factors to come together. Looking | + | Kidney failure while running is extremely rare, and seems to require multiple factors to come together. Looking at the [http://en.wikipedia.org/wiki/Comrades_Marathon Comrades Marathon], a 90 Km/56 Mile ultramarathon in South Africa, there have only been 19 cases of kidney failure between 1969 and 1986, it even though thousands of people participate each year<ref name="rhabdo1"/>. The following are considered factors in acute kidney failure related to running. |
* '''Dehydration'''. Exercise reduces blood flow to the kidneys and dehydration makes this worse. | * '''Dehydration'''. Exercise reduces blood flow to the kidneys and dehydration makes this worse. | ||
| − | * '''NSAIDs'''. NSAIDs also reduce blood flow to the kidneys <ref name="coxibs"/>. NSAIDs reduce prostaglandin production, and prostaglandins are vital to maintaining blood flow to the kidneys. While NSAIDs are considered safe drugs, NSAIDs are associated with a relatively high incidence of adverse drug reactions involving the kidneys. Generally NSAID side effects are restricted to individuals with predisposition to kidney problems, so extra care should be taken if you have a history of kidney problems. However, athletes push their bodies to extremes, so what applies to the general population may not be valid for runners. One runner was told<ref name="Anecdote"/> by doctors that 2400mg Ibuprofen in an ultramarathon was a contributing factor to his kidney failure. | + | * '''NSAIDs'''. NSAIDs also reduce blood flow to the kidneys<ref name="coxibs"/>. NSAIDs reduce prostaglandin production, and prostaglandins are vital to maintaining blood flow to the kidneys. While NSAIDs are considered safe drugs, NSAIDs are associated with a relatively high incidence of adverse drug reactions involving the kidneys. Generally, NSAID side effects are restricted to individuals with predisposition to kidney problems, so extra care should be taken if you have a history of kidney problems. However, athletes push their bodies to extremes, so what applies to the general population may not be valid for runners. One runner was told<ref name="Anecdote"/> by doctors that 2400mg Ibuprofen in an ultramarathon was a contributing factor to his kidney failure. |
| − | * '''Rhabdomyolysis'''. All strenuous exercise causes some muscle damage, but this is generally resolved without a problem. However large amounts of a | + | * '''Rhabdomyolysis'''. All strenuous exercise causes some muscle damage, but this is generally resolved without a problem. However large amounts of a [[Protein]] called myoglobin from damaged muscle can cause a condition called [http://en.wikipedia.org/wiki/Rhabdomyolysis rhabdomyolysis] (AKA 'rhabdo'). While serious rhabdomyolysis is rare, it is worth understanding one key symptom, which is low volume, dark urine, often likened to 'coca-cola'. The other symptoms include severe, incapacitating muscle pain and elevated levels of creatine kinase (CK) in the blood (which requires a specialist test). Some individuals<ref name="rhabdoGenes"/> have a genetic condition that makes rhabdomyolysis possible after relatively moderate exercise. Rhabdomyolysis is also more likely after eccentric exercise, such as [[Downhill Running]]. |
* '''Sickness'''. A viral or bacterial infection is often a factor in exercise related kidney failure. | * '''Sickness'''. A viral or bacterial infection is often a factor in exercise related kidney failure. | ||
| − | Looking at the analysis<ref name="coxibs"/> of nine cases of continued kidney failure in Comrades Marathon, seven had taken NSAIDs, four may have had a viral or bacterial infection. The combination of dehydration, rhabdomyolysis, infection and NSAIDs are a perfect storm for the kidneys. | + | Looking at the analysis<ref name="coxibs"/> of nine cases of continued kidney failure in Comrades Marathon, seven had taken NSAIDs, four may have had a viral or bacterial infection. The combination of dehydration, rhabdomyolysis, infection and NSAIDs are a perfect storm for the kidneys. |
| − | |||
=NSAIDs and Hyponatremia= | =NSAIDs and Hyponatremia= | ||
The kidneys are responsible for removing excess fluid from the blood as well as excreting or withholding sodium. If kidney function is compromised, then this can result in [[Hyponatremia]], which can be fatal. Some studies<ref name="hypo"/><ref name="hypo2"/><ref name="siadh"/> have shown a correlation between NSAID use in races and [[Hyponatremia]], but others<ref name="nohypo"/><ref name="Dumke-2007"/> have not. Using NSAIDs when hydration is a concern increases the risk of problems occuring. | The kidneys are responsible for removing excess fluid from the blood as well as excreting or withholding sodium. If kidney function is compromised, then this can result in [[Hyponatremia]], which can be fatal. Some studies<ref name="hypo"/><ref name="hypo2"/><ref name="siadh"/> have shown a correlation between NSAID use in races and [[Hyponatremia]], but others<ref name="nohypo"/><ref name="Dumke-2007"/> have not. Using NSAIDs when hydration is a concern increases the risk of problems occuring. | ||
| − | + | =NSAIDs causing Heart Attacks or Strokes= | |
| − | =NSAIDs and | + | The U.S. Food and Drug Administration (FDA) warnings that non-aspirin NSAIDs increase the risk of a heart attack or stroke<ref name="www.fda.gov"/>. The risk appears to be related to ongoing usage rather than single doses, with the risk increasing in the first weeks of usage and the risk may increase with prolonged usage. The increased risk is dose dependent (taking more has a greater risk), and the includes those without heart disease or risk factors for heart disease. Not surprisingly, those already with a higher risk of heart disease or stroke have a proportionately higher risk with NSAID usage. |
| + | =NSAIDs and Infection= | ||
Because a bacterial or viral infection puts more stress on the body, including the kidneys, taking NSAIDs and continuing to run increases your risk of complications. If the sickness is too bad to run without NSAIDs, you probably shouldn't run. | Because a bacterial or viral infection puts more stress on the body, including the kidneys, taking NSAIDs and continuing to run increases your risk of complications. If the sickness is too bad to run without NSAIDs, you probably shouldn't run. | ||
| − | |||
=NSAIDs for Pain Reduction= | =NSAIDs for Pain Reduction= | ||
The primary purpose of NSAIDs is generally for reducing pain, and they are remarkably effective at achieving this. If you need a painkiller, acetaminophen is probably a better choice than ibuprofen, though be careful as it's easy to overdose on Acetaminophen (see below). Acetaminophen has limited anti-inflammatory properties, so it shouldn't impair healing as much as ibuprofen, but it is still good as a painkiller. Combining acetaminophen or other NSAIDs with [[Caffeine]] further improves their painkilling effectiveness. After a major race I can sometimes have so much leg pain that I can't [[Zeo Sleep Monitor|sleep]] and a little acetaminophen can make all the difference. While the acetaminophen may impair healing somewhat I believe the trade-off in improved [[Zeo Sleep Monitor|sleep]] is worthwhile. After all, the lack of [[Zeo Sleep Monitor|sleep]] itself will impair healing, so it's a reasonable compromise. | The primary purpose of NSAIDs is generally for reducing pain, and they are remarkably effective at achieving this. If you need a painkiller, acetaminophen is probably a better choice than ibuprofen, though be careful as it's easy to overdose on Acetaminophen (see below). Acetaminophen has limited anti-inflammatory properties, so it shouldn't impair healing as much as ibuprofen, but it is still good as a painkiller. Combining acetaminophen or other NSAIDs with [[Caffeine]] further improves their painkilling effectiveness. After a major race I can sometimes have so much leg pain that I can't [[Zeo Sleep Monitor|sleep]] and a little acetaminophen can make all the difference. While the acetaminophen may impair healing somewhat I believe the trade-off in improved [[Zeo Sleep Monitor|sleep]] is worthwhile. After all, the lack of [[Zeo Sleep Monitor|sleep]] itself will impair healing, so it's a reasonable compromise. | ||
=NSAIDs and DOMS= | =NSAIDs and DOMS= | ||
| − | [[Delayed Onset Muscle Soreness]] (DOMS) generally occurs between 24 and 72 hours after unusual or severe exercise, | + | ''Main article: [[Delayed Onset Muscle Soreness]]'' |
| + | |||
| + | [[Delayed Onset Muscle Soreness]] (DOMS) generally occurs between 24 and 72 hours after unusual or severe exercise, such as racing a marathon or [[Downhill Running]]. The use of NSAIDs to prevent or treat DOMS has been widely researched, with somewhat mixed results. Even scholarly reviews of the research have differing conclusions<ref name="Cheung-2003"/> <ref name="Smith-1992"/> <ref name="Baldwin Lanier-2003"/><ref name="Howatson-2008"/>. My conclusions based on the available research are: | ||
| + | * The most common NSAIDs (Ibuprofen, Acetaminophen (Paracetamol), and Aspirin) are unlikely to help with DOMS. | ||
| + | * There is some evidence that Naproxen may be more effective than the common NSAIDs. There is not enough evidence to reach a conclusion on Diclofenac, Codeine, Rofecoxib, Ketoprofen, or Bromelain. | ||
| + | * There is also some evidence that Turmeric may help with DOMS. | ||
| + | * If an NSAID is taken for DOMS, it should probably be taken immediately after the damaging exercise rather than waiting until the soreness develops. | ||
| + | * It seems likely that taking an NSAID for DOMS will reduce the muscular growth that would normally occur as part of the recovery. In one study, rabbits treated with flurbiprofen after DOMS inducing exercise regained more strength after 3-7 days, but between days 7 and 28 days the treated rabbits became weaker while the controls became stronger<ref name="Mishra-1995"/>. This is only one study, and on animals, but it is rather troubling as none of the human studies look at the results over this time period. | ||
| + | ==A Summary of the Research on NSAIDs and DOMS== | ||
| + | The table below summarizes the research I located on the effect of NSAIDs on DOMS in humans. I've only considered the primary DOMS markers of soreness (pain) and weakness, rather than including things like blood enzymes. For each NSAID I've shown how many studies show an improvement and how many studies show no effect. | ||
| + | {| class="wikitable" | ||
| + | ! NSAID | ||
| + | ! Soreness | ||
| + | ! Weakness | ||
| + | |- | ||
| + | | Ibuprofen | ||
| + | | 2xImproved<ref name="Hasson-1993"/><ref name="pmid12580656"/> | ||
| + | 7xNo Effect<ref name="Grossman-1995"/><ref name="Pizza-1999"/><ref name="RahnamaRahmani-Nia2005"/> <ref name="KrentzQuest2008"/><ref name="Arendt-NielsenWeidner2007"/><ref name="Donnelly-1990"/><ref name="Stone-2002"/> | ||
| + | | 1xMaybe<ref name="Hasson-1993"/> | ||
| + | 8xNo Effect<ref name="Grossman-1995"/><ref name="Pizza-1999"/><ref name="RahnamaRahmani-Nia2005"/> <ref name="KrentzQuest2008"/><ref name="Arendt-NielsenWeidner2007"/><ref name="Donnelly-1990"/><ref name="pmid12580656"/><ref name="Stone-2002"/> | ||
| + | |- | ||
| + | | Ibuprofen Gel | ||
| + | | 1xNo Effect<ref name="HyldahlKeadle2010"/> | ||
| + | | | ||
| + | |- | ||
| + | | Acetaminophen (Paracetamol) | ||
| + | | 2xNo Effect<ref name="Barlas-2000"/><ref name="SmithGeorge1995"/> | ||
| + | | | ||
| + | |- | ||
| + | | Aspirin | ||
| + | | 2xImproved<ref name="Riasata-2010"/><ref name="Francis-1987"/> | ||
| + | 2xNo Effect<ref name="Barlas-2000"/><ref name="SmithGeorge1995"/> | ||
| + | | 2xNo Effect<ref name="Riasata-2010"/><ref name="Francis-1987"/> | ||
| + | |- | ||
| + | | Naproxen | ||
| + | | 4xImproved<ref name="Dudley-1997"/><ref name="Baldwin-2001"/><ref name="Lecomte-1998"/><ref name="journals.ut.ac.ir"/> | ||
| + | 1xNo Effect<ref name="Bourgeois-1999"/> | ||
| + | | 3xImproved<ref name="Dudley-1997"/><ref name="Baldwin-2001"/><ref name="Lecomte-1998"/> | ||
| + | 1xNo Effect<ref name="Bourgeois-1999"/> | ||
| + | |- | ||
| + | | Diclofenac | ||
| + | | Possible slight reduction<ref name="DonnellyMcCormick1988"/> | ||
| + | | | ||
| + | |- | ||
| + | | Codeine | ||
| + | | 1xNo Effect<ref name="Barlas-2000"/> | ||
| + | | | ||
| + | |- | ||
| + | | Rofecoxib | ||
| + | | 1xNo Effect<ref name="LoramMitchell2005"/> | ||
| + | | | ||
| + | |- | ||
| + | | Ketoprofen | ||
| + | | 1xImproved<ref name="Sayers-2001"/> | ||
| + | | 1xImproved<ref name="Sayers-2001"/> | ||
| + | |- | ||
| + | | Bromelain | ||
| + | | 1xNo Effect<ref name="Stone-2002"/> | ||
| + | | | ||
| + | |- | ||
| + | | Turmeric | ||
| + | | 2xImproved<ref name="Nicol-2015"/><ref name="Drobnic-2014"/> | ||
| + | 2xNo Effect<ref name="McFarlinVenable2016"/><ref name="TanabeMaeda2015"/> | ||
| + | | 2xImproved<ref name="TanabeMaeda2015"/><ref name="Davis-2007"/> | ||
| + | |} | ||
=NSAIDs and Intestinal Damage= | =NSAIDs and Intestinal Damage= | ||
| − | As little as one hour of intense cycling can result in indications of small intestinal damage<ref name="van Wijck-2011"/>. This is believed to be due to the redirection of blood away from the digestive system and towards the active muscles. These markers are significantly higher if 400mg ibuprofen (the standard single adult dose) is taken before the exercise<ref name="VAN Wijck-2012"/>. The marker used is Plasma Intestinal Fatty Acid Binding Protein which is an early marker of intestinal necrosis<ref name="Vermeulen Windsant-2012"/>. | + | As little as one hour of intense cycling can result in indications of small intestinal damage<ref name="van Wijck-2011"/>. This is believed to be due to the redirection of blood away from the digestive system and towards the active muscles. These markers are significantly higher if 400mg ibuprofen (the standard single adult dose) is taken before the exercise<ref name="VAN Wijck-2012"/>. The marker used is Plasma Intestinal Fatty Acid Binding [[Protein]] which is an early marker of intestinal necrosis<ref name="Vermeulen Windsant-2012"/>. |
[[File:Ibuprofen and GI damage.jpg|none|thumb|500px|The level of a marker of intestinal damage during and after 60 minutes of cycling at 70% [[VO2max|V̇O<sub>2</sub>max]].]] | [[File:Ibuprofen and GI damage.jpg|none|thumb|500px|The level of a marker of intestinal damage during and after 60 minutes of cycling at 70% [[VO2max|V̇O<sub>2</sub>max]].]] | ||
| + | =NSAIDs and Wound Healing= | ||
| + | ''Main article: [[Popping Blisters]]'' | ||
| + | Ibuprofen, and possibly other NSAIDs, impair wound healing and should be avoided<ref name="StadelmannDigenis1998"/><ref name="GuoDiPietro2010"/>. | ||
=NSAIDs and Racing= | =NSAIDs and Racing= | ||
Taking NSAIDs in ultramarathon events can improve performance by reducing pain and acute inflammation, but doing so represents a significant risk. There is some evidence<ref name="wser1"/> <ref name="wser2"/> that many runners taking NSAIDs have the same level of pain and greater damage markers compared with non-users. This may be because the runners push themselves to a similar level of pain, with the NSAIDs allowing them to do more damage. | Taking NSAIDs in ultramarathon events can improve performance by reducing pain and acute inflammation, but doing so represents a significant risk. There is some evidence<ref name="wser1"/> <ref name="wser2"/> that many runners taking NSAIDs have the same level of pain and greater damage markers compared with non-users. This may be because the runners push themselves to a similar level of pain, with the NSAIDs allowing them to do more damage. | ||
| − | * It seems likely that NSAIDs will increase the risk of injury rather than reducing it, as the symptoms of damage will be masked. | + | * It seems likely that NSAIDs will increase the risk of injury rather than reducing it, as the symptoms of damage will be masked. |
| − | * The most common NSAID for racing seems to be ibuprofen. I've not seen any evidence of the relative effectiveness of different NSAIDs on performance. | + | * The most common NSAID for racing seems to be ibuprofen. I've not seen any evidence of the relative effectiveness of different NSAIDs on performance. |
| − | * It is better to take liquid ibuprofen than tablets or capsules. The tablets and capsules take longer to dissolve and if you have a digestive problem they may not be fully absorbed. You can chew the tablets, but this is unpleasant and ibuprofen can irritate your mouth and throat slightly, so the liquid form is best. It's obviously harder to transport, but you can fill an old film canister with a dose. | + | * It is better to take liquid ibuprofen than tablets or capsules. The tablets and capsules take longer to dissolve and if you have a digestive problem they may not be fully absorbed. You can chew the tablets, but this is unpleasant and ibuprofen can irritate your mouth and throat slightly, so the liquid form is best. It's obviously harder to transport, but you can fill an old film canister with a dose. |
* Before an ultramarathon race, you should think through under what circumstances you will consider using NSAIDs and what dosage. Make sure your crew knows that you're taking NSAIDs in case anything happens. | * Before an ultramarathon race, you should think through under what circumstances you will consider using NSAIDs and what dosage. Make sure your crew knows that you're taking NSAIDs in case anything happens. | ||
* Extra care should be taken when NSAIDs are used in combination with dehydration, sickness or running the causes serious muscle damage. | * Extra care should be taken when NSAIDs are used in combination with dehydration, sickness or running the causes serious muscle damage. | ||
| − | * Taking NSAIDs in marathon or shorter races is probably ineffective as the level of damage seen is not as great as in ultramarathon events. | + | * Taking NSAIDs in marathon or shorter races is probably ineffective as the level of damage seen is not as great as in ultramarathon events. |
* If you need NSAIDs to start a race, you probably should not compete. | * If you need NSAIDs to start a race, you probably should not compete. | ||
=Longer Term NSAID usage= | =Longer Term NSAID usage= | ||
| Line 49: | Line 125: | ||
=Acetaminophen Overdose Danger (AKA Paracetamol, Tylenol)= | =Acetaminophen Overdose Danger (AKA Paracetamol, Tylenol)= | ||
Acetaminophen does not have the same risk of ulcers, but it is linked to liver damage, especially in those who drink alcohol. Acetaminophen is the leading cause of acute liver failure<ref name="AcetaAcuteLiver"/><ref name="Staggered"/>. There are concerns<ref name="AcetaNormalDoseLiver"/> that even the standard dose can cause changes in liver function. Acetaminophen can cause delayed symptoms<ref name="Staggered"/>, with people seeking medical help up to 5 days after the overdose (20% < 12 hours, 35% 12-24 hours, 45% 24 hours+). Overdoses of Acetaminophen can be caused by taking slightly too much over several days, with the toxicity building up<ref name="Staggered"/>. This problem is again exacerbated by those taking alcohol with Acetaminophen<ref name="Staggered"/>. (One factor that increases the risk is that some common medications, such as cold remedies, include Acetaminophen. If people do not add in the dose of Acetaminophen from these other sources, it is easy to unwittingly exceed the safe dosage.) | Acetaminophen does not have the same risk of ulcers, but it is linked to liver damage, especially in those who drink alcohol. Acetaminophen is the leading cause of acute liver failure<ref name="AcetaAcuteLiver"/><ref name="Staggered"/>. There are concerns<ref name="AcetaNormalDoseLiver"/> that even the standard dose can cause changes in liver function. Acetaminophen can cause delayed symptoms<ref name="Staggered"/>, with people seeking medical help up to 5 days after the overdose (20% < 12 hours, 35% 12-24 hours, 45% 24 hours+). Overdoses of Acetaminophen can be caused by taking slightly too much over several days, with the toxicity building up<ref name="Staggered"/>. This problem is again exacerbated by those taking alcohol with Acetaminophen<ref name="Staggered"/>. (One factor that increases the risk is that some common medications, such as cold remedies, include Acetaminophen. If people do not add in the dose of Acetaminophen from these other sources, it is easy to unwittingly exceed the safe dosage.) | ||
| − | = | + | =Is Acetaminophen an NSAID?= |
| − | + | Acetaminophen (also called paracetamol) is generally not classified as an NSAID<ref name="NotAnNsaid"/>. While Acetaminophen has limited anti-inflammatory properties, it shares the same mechanism of action with most NSAIDs of inhibiting the COX enzyme and the inhibition of prostaglandin synthesis<ref name="Graham-2005"/><ref name="BottingAyoub2005"/><ref name="ToussaintYang2010"/><ref name="Anderson2008"/>. Therefore, this article includes Acetaminophen in with NSAIDs. | |
=References= | =References= | ||
<references> | <references> | ||
| + | <ref name="Hawkey1999">CJ Hawkey, COX-2 inhibitors, The Lancet, volume 353, issue 9149, 1999, pages 307–314, ISSN [http://www.worldcat.org/issn/01406736 01406736], doi [http://dx.doi.org/10.1016/S0140-6736(98)12154-2 10.1016/S0140-6736(98)12154-2]</ref> | ||
| + | <ref name="FutakiTakahashi1994">N. Futaki, S. Takahashi, M. Yokoyama, I. Arai, S. Higuchi, S. Otomo, NS-398, a new anti-inflammatory agent, selectively inhibits prostaglandin G/H synthase/cyclooxygenase (COX-2) activity in vitro, Prostaglandins, volume 47, issue 1, 1994, pages 55–59, ISSN [http://www.worldcat.org/issn/00906980 00906980], doi [http://dx.doi.org/10.1016/0090-6980(94)90074-4 10.1016/0090-6980(94)90074-4]</ref> | ||
| + | <ref name="Bertolini-2002">A. Bertolini, A. Ottani, M. Sandrini, Selective COX-2 inhibitors and dual acting anti-inflammatory drugs: critical remarks., Curr Med Chem, volume 9, issue 10, pages 1033-43, May 2002, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12733982 12733982]</ref> | ||
| + | <ref name="Zhu-2014">X. Zhu, Q. Li, R. Chang, D. Yang, Z. Song, Q. Guo, C. Huang, Curcumin alleviates neuropathic pain by inhibiting p300/CBP histone acetyltransferase activity-regulated expression of BDNF and cox-2 in a rat model., PLoS One, volume 9, issue 3, pages e91303, 2014, doi [http://dx.doi.org/10.1371/journal.pone.0091303 10.1371/journal.pone.0091303], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24603592 24603592]</ref> | ||
| + | <ref name="Plummer-1999">SM. Plummer, KA. Holloway, MM. Manson, RJ. Munks, A. Kaptein, S. Farrow, L. Howells, Inhibition of cyclo-oxygenase 2 expression in colon cells by the chemopreventive agent curcumin involves inhibition of NF-kappaB activation via the NIK/IKK signalling complex., Oncogene, volume 18, issue 44, pages 6013-20, Oct 1999, doi [http://dx.doi.org/10.1038/sj.onc.1202980 10.1038/sj.onc.1202980], PMID [http://www.ncbi.nlm.nih.gov/pubmed/10557090 10557090]</ref> | ||
| + | <ref name="Lev-Ari-2006">S. Lev-Ari, A. Starr, A. Vexler, V. Karaush, V. Loew, J. Greif, E. Fenig, D. Aderka, R. Ben-Yosef, Inhibition of pancreatic and lung adenocarcinoma cell survival by curcumin is associated with increased apoptosis, down-regulation of COX-2 and EGFR and inhibition of Erk1/2 activity., Anticancer Res, volume 26, issue 6B, pages 4423-30, PMID [http://www.ncbi.nlm.nih.gov/pubmed/17201164 17201164]</ref> | ||
| + | <ref name="RamsewakDeWitt2000">R.S. Ramsewak, D.L. DeWitt, M.G. Nair, Cytotoxicity, antioxidant and anti-inflammatory activities of Curcumins I–III from Curcuma longa, Phytomedicine, volume 7, issue 4, 2000, pages 303–308, ISSN [http://www.worldcat.org/issn/09447113 09447113], doi [http://dx.doi.org/10.1016/S0944-7113(00)80048-3 10.1016/S0944-7113(00)80048-3]</ref> | ||
| + | <ref name="Ireson-2001">C. Ireson, S. Orr, DJ. Jones, R. Verschoyle, CK. Lim, JL. Luo, L. Howells, S. Plummer, R. Jukes, Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production., Cancer Res, volume 61, issue 3, pages 1058-64, Feb 2001, PMID [http://www.ncbi.nlm.nih.gov/pubmed/11221833 11221833]</ref> | ||
| + | <ref name="Moriyuki-2010">K. Moriyuki, F. Sekiguchi, K. Matsubara, H. Nishikawa, A. Kawabata, Curcumin Inhibits the proteinase-activated receptor-2-triggered prostaglandin E2 production by suppressing cyclooxygenase-2 upregulation and Akt-dependent activation of nuclear factor-κB in human lung epithelial cells., J Pharmacol Sci, volume 114, issue 2, pages 225-9, 2010, PMID [http://www.ncbi.nlm.nih.gov/pubmed/20838026 20838026]</ref> | ||
| + | <ref name="Kawanishi-2013">N. Kawanishi, K. Kato, M. Takahashi, T. Mizokami, Y. Otsuka, A. Imaizumi, D. Shiva, H. Yano, K. Suzuki, Curcumin attenuates oxidative stress following downhill running-induced muscle damage., Biochem Biophys Res Commun, volume 441, issue 3, pages 573-8, Nov 2013, doi [http://dx.doi.org/10.1016/j.bbrc.2013.10.119 10.1016/j.bbrc.2013.10.119], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24184481 24184481]</ref> | ||
| + | <ref name="Davis-2007">JM. Davis, EA. Murphy, MD. Carmichael, MR. Zielinski, CM. Groschwitz, AS. Brown, JD. Gangemi, A. Ghaffar, EP. Mayer, Curcumin effects on inflammation and performance recovery following eccentric exercise-induced muscle damage., Am J Physiol Regul Integr Comp Physiol, volume 292, issue 6, pages R2168-73, Jun 2007, doi [http://dx.doi.org/10.1152/ajpregu.00858.2006 10.1152/ajpregu.00858.2006], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17332159 17332159]</ref> | ||
| + | <ref name="TanabeMaeda2015">Yoko Tanabe, Seiji Maeda, Nobuhiko Akazawa, Asako Zempo-Miyaki, Youngju Choi, Song-Gyu Ra, Atsushi Imaizumi, Yoshihiko Otsuka, Kazunori Nosaka, Attenuation of indirect markers of eccentric exercise-induced muscle damage by curcumin, European Journal of Applied Physiology, volume 115, issue 9, 2015, pages 1949–1957, ISSN [http://www.worldcat.org/issn/1439-6319 1439-6319], doi [http://dx.doi.org/10.1007/s00421-015-3170-4 10.1007/s00421-015-3170-4]</ref> | ||
| + | <ref name="McFarlinVenable2016">Brian K. McFarlin, Adam S. Venable, Andrea L. Henning, Jill N. Best Sampson, Kathryn Pennel, Jakob L. Vingren, David W. Hill, Reduced Inflammatory and Muscle Damage Biomarkers following Oral Supplementation with Bioavailable Curcumin, BBA Clinical, 2016, ISSN [http://www.worldcat.org/issn/22146474 22146474], doi [http://dx.doi.org/10.1016/j.bbacli.2016.02.003 10.1016/j.bbacli.2016.02.003]</ref> | ||
| + | <ref name="Kuptniratsaikul-2014">V. Kuptniratsaikul, P. Dajpratham, W. Taechaarpornkul, M. Buntragulpoontawee, P. Lukkanapichonchut, C. Chootip, J. Saengsuwan, K. Tantayakom, S. Laongpech, Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: a multicenter study., Clin Interv Aging, volume 9, pages 451-8, 2014, doi [http://dx.doi.org/10.2147/CIA.S58535 10.2147/CIA.S58535], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24672232 24672232]</ref> | ||
| + | <ref name="Drobnic-2014">F. Drobnic, J. Riera, G. Appendino, S. Togni, F. Franceschi, X. Valle, A. Pons, J. Tur, Reduction of delayed onset muscle soreness by a novel curcumin delivery system (Meriva): a randomised, placebo-controlled trial., J Int Soc Sports Nutr, volume 11, pages 31, 2014, doi [http://dx.doi.org/10.1186/1550-2783-11-31 10.1186/1550-2783-11-31], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24982601 24982601]</ref> | ||
| + | <ref name="Nicol-2015">LM. Nicol, DS. Rowlands, R. Fazakerly, J. Kellett, Curcumin supplementation likely attenuates delayed onset muscle soreness (DOMS)., Eur J Appl Physiol, volume 115, issue 8, pages 1769-77, Aug 2015, doi [http://dx.doi.org/10.1007/s00421-015-3152-6 10.1007/s00421-015-3152-6], PMID [http://www.ncbi.nlm.nih.gov/pubmed/25795285 25795285]</ref> | ||
| + | <ref name="Henrotin-2014">Y. Henrotin, M. Gharbi, Y. Dierckxsens, F. Priem, M. Marty, L. Seidel, A. Albert, E. Heuse, V. Bonnet, Decrease of a specific biomarker of collagen degradation in osteoarthritis, Coll2-1, by treatment with highly bioavailable curcumin during an exploratory clinical trial., BMC Complement Altern Med, volume 14, pages 159, 2014, doi [http://dx.doi.org/10.1186/1472-6882-14-159 10.1186/1472-6882-14-159], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24886572 24886572]</ref> | ||
| + | <ref name="Chandran-2012">B. Chandran, A. Goel, A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis., Phytother Res, volume 26, issue 11, pages 1719-25, Nov 2012, doi [http://dx.doi.org/10.1002/ptr.4639 10.1002/ptr.4639], PMID [http://www.ncbi.nlm.nih.gov/pubmed/22407780 22407780]</ref> | ||
| + | <ref name="Moini Zanjani-2014">T. Moini Zanjani, H. Ameli, F. Labibi, K. Sedaghat, M. Sabetkasaei, The Attenuation of Pain Behavior and Serum COX-2 Concentration by Curcumin in a Rat Model of Neuropathic Pain., Korean J Pain, volume 27, issue 3, pages 246-52, Jul 2014, doi [http://dx.doi.org/10.3344/kjp.2014.27.3.246 10.3344/kjp.2014.27.3.246], PMID [http://www.ncbi.nlm.nih.gov/pubmed/25031810 25031810]</ref> | ||
| + | <ref name="AppelboomMaes2014">Thierry Appelboom, Nathalie Maes, Adelin Albert, A New Curcuma Extract (Flexofytol®) in Osteoarthritis: Results from a Belgian Real-Life Experience, The Open Rheumatology Journal, volume 8, issue 1, 2014, pages 77–81, ISSN [http://www.worldcat.org/issn/18743129 18743129], doi [http://dx.doi.org/10.2174/1874312901408010077 10.2174/1874312901408010077]</ref> | ||
| + | <ref name="Kuptniratsaikul-2009">V. Kuptniratsaikul, S. Thanakhumtorn, P. Chinswangwatanakul, L. Wattanamongkonsil, V. Thamlikitkul, Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis., J Altern Complement Med, volume 15, issue 8, pages 891-7, Aug 2009, doi [http://dx.doi.org/10.1089/acm.2008.0186 10.1089/acm.2008.0186], PMID [http://www.ncbi.nlm.nih.gov/pubmed/19678780 19678780]</ref> | ||
| + | <ref name="Panahi-2014">Y. Panahi, AR. Rahimnia, M. Sharafi, G. Alishiri, A. Saburi, A. Sahebkar, Curcuminoid treatment for knee osteoarthritis: a randomized double-blind placebo-controlled trial., Phytother Res, volume 28, issue 11, pages 1625-31, Nov 2014, doi [http://dx.doi.org/10.1002/ptr.5174 10.1002/ptr.5174], PMID [http://www.ncbi.nlm.nih.gov/pubmed/24853120 24853120]</ref> | ||
| + | <ref name="Agarwal-2011">KA. Agarwal, CD. Tripathi, BB. Agarwal, S. Saluja, Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study., Surg Endosc, volume 25, issue 12, pages 3805-10, Dec 2011, doi [http://dx.doi.org/10.1007/s00464-011-1793-z 10.1007/s00464-011-1793-z], PMID [http://www.ncbi.nlm.nih.gov/pubmed/21671126 21671126]</ref> | ||
| + | <ref name="AnandKunnumakkara2007">Preetha Anand, Ajaikumar B. Kunnumakkara, Robert A. Newman, Bharat B. Aggarwal, Bioavailability of Curcumin: Problems and Promises, Molecular Pharmaceutics, volume 4, issue 6, 2007, pages 807–818, ISSN [http://www.worldcat.org/issn/1543-8384 1543-8384], doi [http://dx.doi.org/10.1021/mp700113r 10.1021/mp700113r]</ref> | ||
| + | <ref name="Cheng-2001">AL. Cheng, CH. Hsu, JK. Lin, MM. Hsu, YF. Ho, TS. Shen, JY. Ko, JT. Lin, BR. Lin, Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions., Anticancer Res, volume 21, issue 4B, pages 2895-900, PMID [http://www.ncbi.nlm.nih.gov/pubmed/11712783 11712783]</ref> | ||
| + | <ref name="Hsu-2007">CH. Hsu, AL. Cheng, Clinical studies with curcumin., Adv Exp Med Biol, volume 595, pages 471-80, 2007, doi [http://dx.doi.org/10.1007/978-0-387-46401-5_21 10.1007/978-0-387-46401-5_21], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17569225 17569225]</ref> | ||
| + | <ref name="Henrotin-2010">Y. Henrotin, AL. Clutterbuck, D. Allaway, EM. Lodwig, P. Harris, M. Mathy-Hartert, M. Shakibaei, A. Mobasheri, Biological actions of curcumin on articular chondrocytes., Osteoarthritis Cartilage, volume 18, issue 2, pages 141-9, Feb 2010, doi [http://dx.doi.org/10.1016/j.joca.2009.10.002 10.1016/j.joca.2009.10.002], PMID [http://www.ncbi.nlm.nih.gov/pubmed/19836480 19836480]</ref> | ||
| + | <ref name="Anand-2010">P. Anand, HB. Nair, B. Sung, AB. Kunnumakkara, VR. Yadav, RR. Tekmal, BB. Aggarwal, Design of curcumin-loaded PLGA nanoparticles formulation with enhanced cellular uptake, and increased bioactivity in vitro and superior bioavailability in vivo., Biochem Pharmacol, volume 79, issue 3, pages 330-8, Feb 2010, doi [http://dx.doi.org/10.1016/j.bcp.2009.09.003 10.1016/j.bcp.2009.09.003], PMID [http://www.ncbi.nlm.nih.gov/pubmed/19735646 19735646]</ref> | ||
| + | <ref name="PanahiSahebkar2012">Y. Panahi, A. Sahebkar, S. Parvin, A. Saadat, A randomized controlled trial on the anti-inflammatory effects of curcumin in patients with chronic sulphur mustard-induced cutaneous complications, Annals of Clinical Biochemistry, volume 49, issue 6, 2012, pages 580–588, ISSN [http://www.worldcat.org/issn/0004-5632 0004-5632], doi [http://dx.doi.org/10.1258/acb.2012.012040 10.1258/acb.2012.012040]</ref> | ||
| + | <ref name="Sahebkar2014">Amirhossein Sahebkar, Are Curcuminoids Effective C-Reactive Protein-Lowering Agents in Clinical Practice? Evidence from a Meta-Analysis, Phytotherapy Research, volume 28, issue 5, 2014, pages 633–642, ISSN [http://www.worldcat.org/issn/0951418X 0951418X], doi [http://dx.doi.org/10.1002/ptr.5045 10.1002/ptr.5045]</ref> | ||
<ref name="bone">JBJS | Dose and Time-Dependent Effects of Cyclooxygenase-2 Inhibition on Fracture-Healing http://www.jbjs.org/article.aspx?Volume=89&page=500</ref> | <ref name="bone">JBJS | Dose and Time-Dependent Effects of Cyclooxygenase-2 Inhibition on Fracture-Healing http://www.jbjs.org/article.aspx?Volume=89&page=500</ref> | ||
<ref name="tendon">NSAIDs Inhibit Tendon-to-Bone Healing in Rotator Cuff Repair http://www.shoulderdoc.co.uk/article.asp?article=295</ref> | <ref name="tendon">NSAIDs Inhibit Tendon-to-Bone Healing in Rotator Cuff Repair http://www.shoulderdoc.co.uk/article.asp?article=295</ref> | ||
| Line 82: | Line 188: | ||
<ref name="rhabdoGenes">Recurrent rhabdomyolysis in a collegiat... [Med Sci Sports Exerc. 2006] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16540825</ref> | <ref name="rhabdoGenes">Recurrent rhabdomyolysis in a collegiat... [Med Sci Sports Exerc. 2006] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16540825</ref> | ||
<ref name="siadh"> http://www.sciencedirect.com/science/article/pii/S0002934307001672</ref> | <ref name="siadh"> http://www.sciencedirect.com/science/article/pii/S0002934307001672</ref> | ||
| − | <ref name=" | + | <ref name="Dumke-2007">CL. Dumke, DC. Nieman, K. Oley, RH. Lind, Ibuprofen does not affect serum electrolyte concentrations after an ultradistance run., Br J Sports Med, volume 41, issue 8, pages 492-6; discussion 496, Aug 2007, doi [http://dx.doi.org/10.1136/bjsm.2006.033597 10.1136/bjsm.2006.033597], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17331976 17331976]</ref> |
| − | + | <ref name="VAN Wijck-2012"> K. VAN Wijck, K. Lenaerts, AA. VAN Bijnen, B. Boonen, LJ. VAN Loon, CH. Dejong, WA. Buurman, Aggravation of exercise-induced intestinal injury by Ibuprofen in athletes., Med Sci Sports Exerc, volume 44, issue 12, pages 2257-62, Dec 2012, doi [http://dx.doi.org/10.1249/MSS.0b013e318265dd3d 10.1249/MSS.0b013e318265dd3d], PMID [http://www.ncbi.nlm.nih.gov/pubmed/22776871 22776871]</ref> | |
| − | + | <ref name="van Wijck-2011"> K. van Wijck, K. Lenaerts, LJ. van Loon, WH. Peters, WA. Buurman, CH. Dejong, Exercise-induced splanchnic hypoperfusion results in gut dysfunction in healthy men., PLoS One, volume 6, issue 7, pages e22366, 2011, doi [http://dx.doi.org/10.1371/journal.pone.0022366 10.1371/journal.pone.0022366], PMID [http://www.ncbi.nlm.nih.gov/pubmed/21811592 21811592]</ref> | |
| − | + | <ref name="Vermeulen Windsant-2012"> IC. Vermeulen Windsant, FA. Hellenthal, JP. Derikx, MH. Prins, WA. Buurman, MJ. Jacobs, GW. Schurink, Circulating intestinal fatty acid-binding protein as an early marker of intestinal necrosis after aortic surgery: a prospective observational cohort study., Ann Surg, volume 255, issue 4, pages 796-803, Apr 2012, doi [http://dx.doi.org/10.1097/SLA.0b013e31824b1e16 10.1097/SLA.0b013e31824b1e16], PMID [http://www.ncbi.nlm.nih.gov/pubmed/22367448 22367448]</ref> | |
| − | <ref name="van Wijck-2011"> | + | <ref name="Riasata-2010">Riasati et al.: Aspirin and delayed onset muscle soreness ASPIRIN MAY BE AN EFFECTIVE TREATMENT FOR EXERCISE- INDUCED MUSCLE SORENESS | ResearchGate http://www.researchgate.net/publication/228091056_Riasati_et_al._Aspirin_and_delayed_onset_muscle_soreness_ASPIRIN_MAY_BE_AN_EFFECTIVE_TREATMENT_FOR_EXERCISE-_INDUCED_MUSCLE_SORENESS </ref> |
| − | <ref name="Vermeulen Windsant-2012"> | + | <ref name="Francis-1987"> KT. Francis, T. Hoobler, Effects of aspirin on delayed muscle soreness., J Sports Med Phys Fitness, volume 27, issue 3, pages 333-7, Sep 1987, PMID [http://www.ncbi.nlm.nih.gov/pubmed/3431117 3431117]</ref> |
| + | <ref name="Donnelly-1990"> AE. Donnelly, RJ. Maughan, PH. Whiting, Effects of ibuprofen on exercise-induced muscle soreness and indices of muscle damage., Br J Sports Med, volume 24, issue 3, pages 191-5, Sep 1990, PMID [http://www.ncbi.nlm.nih.gov/pubmed/2078806 2078806]</ref> | ||
| + | <ref name="DonnellyMcCormick1988">A E Donnelly, K McCormick, R J Maughan, P H Whiting, P M Clarkson, Effects of a non-steroidal anti-inflammatory drug on delayed onset muscle soreness and indices of damage., British Journal of Sports Medicine, volume 22, issue 1, 1988, pages 35–38, ISSN [http://www.worldcat.org/issn/0306-3674 0306-3674], doi [http://dx.doi.org/10.1136/bjsm.22.1.35 10.1136/bjsm.22.1.35]</ref> | ||
| + | <ref name="Hasson-1993"> SM. Hasson, JC. Daniels, JG. Divine, BR. Niebuhr, S. Richmond, PG. Stein, JH. Williams, Effect of ibuprofen use on muscle soreness, damage, and performance: a preliminary investigation., Med Sci Sports Exerc, volume 25, issue 1, pages 9-17, Jan 1993, PMID [http://www.ncbi.nlm.nih.gov/pubmed/8423760 8423760]</ref> | ||
| + | <ref name="Grossman-1995">Effect of Ibuprofen Use on Delayed Onset Muscle Soreness of the Elbow Flexors http://journals.humankinetics.com/jsr-back-issues/jsrvolume4issue4november/effectofibuprofenuseondelayedonsetmusclesorenessoftheelbowflexors </ref> | ||
| + | <ref name="Dudley-1997"> GA. Dudley, J. Czerkawski, A. Meinrod, G. Gillis, A. Baldwin, M. Scarpone, Efficacy of naproxen sodium for exercise-induced dysfunction muscle injury and soreness., Clin J Sport Med, volume 7, issue 1, pages 3-10, Jan 1997, PMID [http://www.ncbi.nlm.nih.gov/pubmed/9117523 9117523]</ref> | ||
| + | <ref name="Barlas-2000"> P. Barlas, JA. Craig, J. Robinson, DM. Walsh, GD. Baxter, JM. Allen, Managing delayed-onset muscle soreness: lack of effect of selected oral systemic analgesics., Arch Phys Med Rehabil, volume 81, issue 7, pages 966-72, Jul 2000, doi [http://dx.doi.org/10.1053/apmr.2000.6277 10.1053/apmr.2000.6277], PMID [http://www.ncbi.nlm.nih.gov/pubmed/10896014 10896014]</ref> | ||
| + | <ref name="Pizza-1999"> FX. Pizza, D. Cavender, A. Stockard, H. Baylies, A. Beighle, Anti-inflammatory doses of ibuprofen: effect on neutrophils and exercise-induced muscle injury., Int J Sports Med, volume 20, issue 2, pages 98-102, Feb 1999, doi [http://dx.doi.org/10.1055/s-2007-971100 10.1055/s-2007-971100], PMID [http://www.ncbi.nlm.nih.gov/pubmed/10190769 10190769]</ref> | ||
| + | <ref name="SmithGeorge1995">Lucille Smith, Robert George, Thomas Chenier, Michael McCammon, Joseph Houmard, Richard Israel, R. A. Hoppmann, Susan Smith, Do over-the-counter analgesics reduce delayed onset muscle soreness and serum creatine kinase values?, Research in Sports Medicine, volume 6, issue 2, 1995, pages 81–88, ISSN [http://www.worldcat.org/issn/1543-8627 1543-8627], doi [http://dx.doi.org/10.1080/15438629509512039 10.1080/15438629509512039]</ref> | ||
| + | <ref name="Baldwin-2001"> AC. Baldwin, SW. Stevenson, GA. Dudley, Nonsteroidal anti-inflammatory therapy after eccentric exercise in healthy older individuals., J Gerontol A Biol Sci Med Sci, volume 56, issue 8, pages M510-3, Aug 2001, PMID [http://www.ncbi.nlm.nih.gov/pubmed/11487604 11487604]</ref> | ||
| + | <ref name="pmid12580656">Tokmakidis SP, Kokkinidis EA, Smilios I, Douda H, The effects of ibuprofen on delayed muscle soreness and muscular performance after eccentric exercise., J Strength Cond Res, 2003, volume 17, issue 1, pages 53-9, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12580656 12580656] </ref> | ||
| + | <ref name="Stone-2002"> MB. Stone, MA. Merrick, CD. Ingersoll, JE. Edwards, Preliminary comparison of bromelain and Ibuprofen for delayed onset muscle soreness management., Clin J Sport Med, volume 12, issue 6, pages 373-8, Nov 2002, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12466693 12466693]</ref> | ||
| + | <ref name="RahnamaRahmani-Nia2005">N Rahnama, F Rahmani-Nia, K Ebrahim, The isolated and combined effects of selected physical activity and ibuprofen on delayed-onset muscle soreness, Journal of Sports Sciences, volume 23, issue 8, 2005, pages 843–850, ISSN [http://www.worldcat.org/issn/0264-0414 0264-0414], doi [http://dx.doi.org/10.1080/02640410400021989 10.1080/02640410400021989]</ref> | ||
| + | <ref name="KrentzQuest2008">Joel R. Krentz, Braden Quest, Jonathan P. Farthing, Dale W. Quest, Philip D. Chilibeck, The effects of ibuprofen on muscle hypertrophy, strength, and soreness during resistance training, Applied Physiology, Nutrition, and Metabolism, volume 33, issue 3, 2008, pages 470–475, ISSN [http://www.worldcat.org/issn/1715-5312 1715-5312], doi [http://dx.doi.org/10.1139/H08-019 10.1139/H08-019]</ref> | ||
| + | <ref name="HyldahlKeadle2010">Robert D. Hyldahl, Justin Keadle, Pierre A. Rouzier, Dennis Pearl, Priscilla M. Clarkson, Effects of Ibuprofen Topical Gel on Muscle Soreness, Medicine & Science in Sports & Exercise, volume 42, issue 3, 2010, pages 614–621, ISSN [http://www.worldcat.org/issn/0195-9131 0195-9131], doi [http://dx.doi.org/10.1249/MSS.0b013e3181b95db2 10.1249/MSS.0b013e3181b95db2]</ref> | ||
| + | <ref name="Arendt-NielsenWeidner2007">Lars Arendt-Nielsen, Morten Weidner, Dorte Bartholin, Allan Rosetzsky, A Double-Blind Randomized Placebo Controlled Parallel Group Study Evaluating the Effects of Ibuprofen and Glucosamine Sulfate on Exercise Induced Muscle Soreness, Journal Of Musculoskeletal Pain, volume 15, issue 1, 2007, pages 21–28, ISSN [http://www.worldcat.org/issn/1058-2452 1058-2452], doi [http://dx.doi.org/10.1300/J094v15n01_04 10.1300/J094v15n01_04]</ref> | ||
| + | <ref name="LoramMitchell2005">L.C. Loram, D. Mitchell, A. Fuller, Rofecoxib and tramadol do not attenuate delayed-onset muscle soreness or ischaemic pain in human volunteers, Canadian Journal of Physiology and Pharmacology, volume 83, issue 12, 2005, pages 1137–1145, ISSN [http://www.worldcat.org/issn/0008-4212 0008-4212], doi [http://dx.doi.org/10.1139/y05-113 10.1139/y05-113]</ref> | ||
| + | <ref name="Howatson-2008"> G. Howatson, KA. van Someren, The prevention and treatment of exercise-induced muscle damage., Sports Med, volume 38, issue 6, pages 483-503, 2008, PMID [http://www.ncbi.nlm.nih.gov/pubmed/18489195 18489195]</ref> | ||
| + | <ref name="Lecomte-1998"> JM. Lecomte, VJ. Lacroix, DL. Montgomery, A randomized controlled trial of the effect of naproxen on delayed onset muscle soreness and muscle strength., Clin J Sport Med, volume 8, issue 2, pages 82-7, Apr 1998, PMID [http://www.ncbi.nlm.nih.gov/pubmed/9641434 9641434]</ref> | ||
| + | <ref name="Mishra-1995"> DK. Mishra, J. Fridén, MC. Schmitz, RL. Lieber, Anti-inflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function., J Bone Joint Surg Am, volume 77, issue 10, pages 1510-9, Oct 1995, PMID [http://www.ncbi.nlm.nih.gov/pubmed/7593059 7593059]</ref> | ||
| + | <ref name="Sayers-2001"> SP. Sayers, CA. Knight, PM. Clarkson, EH. Van Wegen, G. Kamen, Effect of ketoprofen on muscle function and sEMG activity after eccentric exercise., Med Sci Sports Exerc, volume 33, issue 5, pages 702-10, May 2001, PMID [http://www.ncbi.nlm.nih.gov/pubmed/11323536 11323536]</ref> | ||
| + | <ref name="Bourgeois-1999"> J. Bourgeois, D. MacDougall, J. MacDonald, M. Tarnopolsky, Naproxen does not alter indices of muscle damage in resistance-exercise trained men., Med Sci Sports Exerc, volume 31, issue 1, pages 4-9, Jan 1999, PMID [http://www.ncbi.nlm.nih.gov/pubmed/9927002 9927002]</ref> | ||
| + | <ref name="journals.ut.ac.ir"> The Effect of Taking Naproxen Drug on the Level of Perceived Pain and Changes of CPK Serum after Eccentric Exercise - Harakat Volume: 37, Issue:, Accessed on 3 January 2013</ref> | ||
| + | <ref name="Cheung-2003"> K. Cheung, P. Hume, L. Maxwell, Delayed onset muscle soreness : treatment strategies and performance factors., Sports Med, volume 33, issue 2, pages 145-64, 2003, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12617692 12617692]</ref> | ||
| + | <ref name="Smith-1992"> Smith LL. Causes of delayed onset muscle soreness and the impact on athletic performance: a review. J Appl Sport Sci Res 1992; 6 (3): 135-41</ref> | ||
| + | <ref name="Baldwin Lanier-2003"> A. Baldwin Lanier, Use of nonsteroidal anti-inflammatory drugs following exercise-induced muscle injury., Sports Med, volume 33, issue 3, pages 177-85, 2003, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12656639 12656639]</ref> | ||
| + | <ref name="StadelmannDigenis1998">Wayne K. Stadelmann, Alexander G. Digenis, Gordon R. Tobin, Impediments to wound healing, The American Journal of Surgery, volume 176, issue 2, 1998, pages 39S–47S, ISSN [http://www.worldcat.org/issn/00029610 00029610], doi [http://dx.doi.org/10.1016/S0002-9610(98)00184-6 10.1016/S0002-9610(98)00184-6]</ref> | ||
| + | <ref name="GuoDiPietro2010">S. Guo, L. A. DiPietro, Factors Affecting Wound Healing, Journal of Dental Research, volume 89, issue 3, 2010, pages 219–229, ISSN [http://www.worldcat.org/issn/0022-0345 0022-0345], doi [http://dx.doi.org/10.1177/0022034509359125 10.1177/0022034509359125]</ref> | ||
| + | <ref name="Graham-2005">GG. Graham, KF. Scott, Mechanism of action of paracetamol., Am J Ther, volume 12, issue 1, pages 46-55, PMID [http://www.ncbi.nlm.nih.gov/pubmed/15662292 15662292]</ref> | ||
| + | <ref name="Anderson2008">Brian J. Anderson, Paracetamol (Acetaminophen): mechanisms of action, Pediatric Anesthesia, volume 18, issue 10, 2008, pages 915–921, ISSN [http://www.worldcat.org/issn/11555645 11555645], doi [http://dx.doi.org/10.1111/j.1460-9592.2008.02764.x 10.1111/j.1460-9592.2008.02764.x]</ref> | ||
| + | <ref name="BottingAyoub2005">Regina Botting, Samir S. Ayoub, COX-3 and the mechanism of action of paracetamol/acetaminophen, Prostaglandins, Leukotrienes and Essential Fatty Acids, volume 72, issue 2, 2005, pages 85–87, ISSN [http://www.worldcat.org/issn/09523278 09523278], doi [http://dx.doi.org/10.1016/j.plefa.2004.10.005 10.1016/j.plefa.2004.10.005]</ref> | ||
| + | <ref name="ToussaintYang2010">K. Toussaint, X. C. Yang, M. A. Zielinski, K. L. Reigle, S. D. Sacavage, S. Nagar, R. B. Raffa, What do we (not) know about how paracetamol (acetaminophen) works?, Journal of Clinical Pharmacy and Therapeutics, volume 35, issue 6, 2010, pages 617–638, ISSN [http://www.worldcat.org/issn/02694727 02694727], doi [http://dx.doi.org/10.1111/j.1365-2710.2009.01143.x 10.1111/j.1365-2710.2009.01143.x]</ref> | ||
| + | <ref name="www.fda.gov">FDA Drug Safety Communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes, http://www.fda.gov/Drugs/DrugSafety/ucm451800.htm, Accessed on 25 January 2016</ref> | ||
| + | <ref name="JoslinLloyd2013">Jeremy D Joslin, Jarem B Lloyd, Timur Kotlyar, Susan M Wojcik, NSAID and other analgesic use by endurance runners during training, competition and recovery, South African Journal of Sports Medicine, volume 25, issue 4, 2013, pages 101, ISSN [http://www.worldcat.org/issn/2078-516X 2078-516X], doi [http://dx.doi.org/10.7196/sajsm.495 10.7196/sajsm.495]</ref> | ||
| + | <ref name="vanGent-2007">RN. van Gent, D. Siem, M. van Middelkoop, AG. van Os, SM. Bierma-Zeinstra, BW. Koes, Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review., Br J Sports Med, volume 41, issue 8, pages 469-80; discussion 480, Aug 2007, doi [http://dx.doi.org/10.1136/bjsm.2006.033548 10.1136/bjsm.2006.033548], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17473005 17473005]</ref> | ||
| + | <ref name="Benzie-">IFF. Benzie, S. Wachtel-Galor, S. Prasad, BB. Aggarwal, Turmeric, the Golden Spice: From Traditional Medicine to Modern Medicine, PMID [http://www.ncbi.nlm.nih.gov/pubmed/22593922 22593922]</ref> | ||
| + | <ref name="GanigerMalleshappa2007">S. Ganiger, H.N. Malleshappa, H. Krishnappa, Geetha Rajashekhar, V. Ramakrishna Rao, Frank Sullivan, A two generation reproductive toxicity study with curcumin, turmeric yellow, in Wistar rats, Food and Chemical Toxicology, volume 45, issue 1, 2007, pages 64–69, ISSN [http://www.worldcat.org/issn/02786915 02786915], doi [http://dx.doi.org/10.1016/j.fct.2006.07.016 10.1016/j.fct.2006.07.016]</ref> | ||
| + | <ref name="Hawkey-2001">CJ. Hawkey, COX-1 and COX-2 inhibitors., Best Pract Res Clin Gastroenterol, volume 15, issue 5, pages 801-20, Oct 2001, doi [http://dx.doi.org/10.1053/bega.2001.0236 10.1053/bega.2001.0236], PMID [http://www.ncbi.nlm.nih.gov/pubmed/11566042 11566042]</ref> | ||
| + | <ref name="RaoDinkar2013">S. Rao, C. Dinkar, L. K. Vaishnav, P. Rao, M. P. Rai, R. Fayad, M. S. Baliga, The Indian Spice Turmeric Delays and Mitigates Radiation-Induced Oral Mucositis in Patients Undergoing Treatment for Head and Neck Cancer: An Investigational Study, Integrative Cancer Therapies, volume 13, issue 3, 2013, pages 201–210, ISSN [http://www.worldcat.org/issn/1534-7354 1534-7354], doi [http://dx.doi.org/10.1177/1534735413503549 10.1177/1534735413503549]</ref> | ||
| + | <ref name="Gupta-2013">SC. Gupta, S. Patchva, BB. Aggarwal, Therapeutic roles of curcumin: lessons learned from clinical trials., AAPS J, volume 15, issue 1, pages 195-218, Jan 2013, doi [http://dx.doi.org/10.1208/s12248-012-9432-8 10.1208/s12248-012-9432-8], PMID [http://www.ncbi.nlm.nih.gov/pubmed/23143785 23143785]</ref> | ||
| + | <ref name="Shah-1999">BH. Shah, Z. Nawaz, SA. Pertani, A. Roomi, H. Mahmood, SA. Saeed, AH. Gilani, Inhibitory effect of curcumin, a food spice from turmeric, on platelet-activating factor- and arachidonic acid-mediated platelet aggregation through inhibition of thromboxane formation and Ca2+ signaling., Biochem Pharmacol, volume 58, issue 7, pages 1167-72, Oct 1999, PMID [http://www.ncbi.nlm.nih.gov/pubmed/10484074 10484074]</ref> | ||
| + | <ref name="Goodman-2004">GE. Goodman, MD. Thornquist, J. Balmes, MR. Cullen, FL. Meyskens, GS. Omenn, B. Valanis, JH. Williams, The Beta-Carotene and Retinol Efficacy Trial: incidence of lung cancer and cardiovascular disease mortality during 6-year follow-up after stopping beta-carotene and retinol supplements., J Natl Cancer Inst, volume 96, issue 23, pages 1743-50, Dec 2004, doi [http://dx.doi.org/10.1093/jnci/djh320 10.1093/jnci/djh320], PMID [http://www.ncbi.nlm.nih.gov/pubmed/15572756 15572756]</ref> | ||
| + | <ref name="Sharma-2005">RA. Sharma, AJ. Gescher, WP. Steward, Curcumin: the story so far., Eur J Cancer, volume 41, issue 13, pages 1955-68, Sep 2005, doi [http://dx.doi.org/10.1016/j.ejca.2005.05.009 10.1016/j.ejca.2005.05.009], PMID [http://www.ncbi.nlm.nih.gov/pubmed/16081279 16081279]</ref> | ||
| + | <ref name="Means2008">R. T. Means, Ironing out complementary medicine, Blood, volume 113, issue 2, 2008, pages 270–271, ISSN [http://www.worldcat.org/issn/0006-4971 0006-4971], doi [http://dx.doi.org/10.1182/blood-2008-10-184630 10.1182/blood-2008-10-184630]</ref> | ||
| + | <ref name="Baum-2004">L. Baum, A. Ng, Curcumin interaction with copper and iron suggests one possible mechanism of action in Alzheimer's disease animal models., J Alzheimers Dis, volume 6, issue 4, pages 367-77; discussion 443-9, Aug 2004, PMID [http://www.ncbi.nlm.nih.gov/pubmed/15345806 15345806]</ref> | ||
| + | <ref name="Jiao-2009">Y. Jiao, J. Wilkinson, X. Di, W. Wang, H. Hatcher, ND. Kock, R. D'Agostino, MA. Knovich, FM. Torti, Curcumin, a cancer chemopreventive and chemotherapeutic agent, is a biologically active iron chelator., Blood, volume 113, issue 2, pages 462-9, Jan 2009, doi [http://dx.doi.org/10.1182/blood-2008-05-155952 10.1182/blood-2008-05-155952], PMID [http://www.ncbi.nlm.nih.gov/pubmed/18815282 18815282]</ref> | ||
| + | <ref name="López-Lázaro-2008">M. López-Lázaro, Anticancer and carcinogenic properties of curcumin: considerations for its clinical development as a cancer chemopreventive and chemotherapeutic agent., Mol Nutr Food Res, volume 52 Suppl 1, pages S103-27, Jun 2008, doi [http://dx.doi.org/10.1002/mnfr.200700238 10.1002/mnfr.200700238], PMID [http://www.ncbi.nlm.nih.gov/pubmed/18496811 18496811]</ref> | ||
| + | <ref name="Urbina-Cano-2006">P. Urbina-Cano, L. Bobadilla-Morales, MA. Ramírez-Herrera, JR. Corona-Rivera, ML. Mendoza-Magaña, R. Troyo-Sanromán, A. Corona-Rivera, DNA damage in mouse lymphocytes exposed to curcumin and copper., J Appl Genet, volume 47, issue 4, pages 377-82, 2006, doi [http://dx.doi.org/10.1007/BF03194648 10.1007/BF03194648], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17132903 17132903]</ref> | ||
| + | <ref name="Cao-2006">J. Cao, L. Jia, HM. Zhou, Y. Liu, LF. Zhong, Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells., Toxicol Sci, volume 91, issue 2, pages 476-83, Jun 2006, doi [http://dx.doi.org/10.1093/toxsci/kfj153 10.1093/toxsci/kfj153], PMID [http://www.ncbi.nlm.nih.gov/pubmed/16537656 16537656]</ref> | ||
| + | <ref name="Kelly-2001">MR. Kelly, J. Xu, KE. Alexander, G. Loo, Disparate effects of similar phenolic phytochemicals as inhibitors of oxidative damage to cellular DNA., Mutat Res, volume 485, issue 4, pages 309-18, May 2001, PMID [http://www.ncbi.nlm.nih.gov/pubmed/11585363 11585363]</ref> | ||
| + | <ref name="Blasiak-1999">J. Blasiak, A. Trzeciak, J. Kowalik, Curcumin damages DNA in human gastric mucosa cells and lymphocytes., J Environ Pathol Toxicol Oncol, volume 18, issue 4, pages 271-6, 1999, PMID [http://www.ncbi.nlm.nih.gov/pubmed/15281237 15281237]</ref> | ||
| + | <ref name="Nair-2005">J. Nair, S. Strand, N. Frank, J. Knauft, H. Wesch, PR. Galle, H. Bartsch, Apoptosis and age-dependant induction of nuclear and mitochondrial etheno-DNA adducts in Long-Evans Cinnamon (LEC) rats: enhanced DNA damage by dietary curcumin upon copper accumulation., Carcinogenesis, volume 26, issue 7, pages 1307-15, Jul 2005, doi [http://dx.doi.org/10.1093/carcin/bgi073 10.1093/carcin/bgi073], PMID [http://www.ncbi.nlm.nih.gov/pubmed/15790590 15790590]</ref> | ||
| + | <ref name="Sakano-2002">K. Sakano, S. Kawanishi, Metal-mediated DNA damage induced by curcumin in the presence of human cytochrome P450 isozymes., Arch Biochem Biophys, volume 405, issue 2, pages 223-30, Sep 2002, PMID [http://www.ncbi.nlm.nih.gov/pubmed/12220536 12220536]</ref> | ||
| + | <ref name="Ahsan-1998">H. Ahsan, SM. Hadi, Strand scission in DNA induced by curcumin in the presence of Cu(II)., Cancer Lett, volume 124, issue 1, pages 23-30, Feb 1998, PMID [http://www.ncbi.nlm.nih.gov/pubmed/9500187 9500187]</ref> | ||
| + | <ref name="Giri-1990">AK. Giri, SK. Das, G. Talukder, A. Sharma, Sister chromatid exchange and chromosome aberrations induced by curcumin and tartrazine on mammalian cells in vivo., Cytobios, volume 62, issue 249, pages 111-7, 1990, PMID [http://www.ncbi.nlm.nih.gov/pubmed/2209081 2209081]</ref> | ||
| + | <ref name="GoodpastureArrighi1976">C.E. Goodpasture, F.E. Arrighi, Effects of food seasonings on the cell cycle and chromosome morphology of mammalian cells in vitro with special reference to turmeric, Food and Cosmetics Toxicology, volume 14, issue 1, 1976, pages 9–14, ISSN [http://www.worldcat.org/issn/00156264 00156264], doi [http://dx.doi.org/10.1016/S0015-6264(76)80356-2 10.1016/S0015-6264(76)80356-2]</ref> | ||
| + | <ref name="Bhardwaj-2002">RK. Bhardwaj, H. Glaeser, L. Becquemont, U. Klotz, SK. Gupta, MF. Fromm, Piperine, a major constituent of black pepper, inhibits human P-glycoprotein and CYP3A4., J Pharmacol Exp Ther, volume 302, issue 2, pages 645-50, Aug 2002, doi [http://dx.doi.org/10.1124/jpet.102.034728 10.1124/jpet.102.034728], PMID [http://www.ncbi.nlm.nih.gov/pubmed/12130727 12130727]</ref> | ||
| + | <ref name="Atal-1985">CK. Atal, RK. Dubey, J. Singh, Biochemical basis of enhanced drug bioavailability by piperine: evidence that piperine is a potent inhibitor of drug metabolism., J Pharmacol Exp Ther, volume 232, issue 1, pages 258-62, Jan 1985, PMID [http://www.ncbi.nlm.nih.gov/pubmed/3917507 3917507]</ref> | ||
| + | <ref name="Mancuso-2009">C. Mancuso, E. Barone, Curcumin in clinical practice: myth or reality?, Trends Pharmacol Sci, volume 30, issue 7, pages 333-4, Jul 2009, doi [http://dx.doi.org/10.1016/j.tips.2009.04.004 10.1016/j.tips.2009.04.004], PMID [http://www.ncbi.nlm.nih.gov/pubmed/19523696 19523696]</ref> | ||
| + | <ref name="Volak-2008">LP. Volak, S. Ghirmai, JR. Cashman, MH. Court, Curcuminoids inhibit multiple human cytochromes P450, UDP-glucuronosyltransferase, and sulfotransferase enzymes, whereas piperine is a relatively selective CYP3A4 inhibitor., Drug Metab Dispos, volume 36, issue 8, pages 1594-605, Aug 2008, doi [http://dx.doi.org/10.1124/dmd.108.020552 10.1124/dmd.108.020552], PMID [http://www.ncbi.nlm.nih.gov/pubmed/18480186 18480186]</ref> | ||
| + | <ref name="Appiah-Opong-2007">R. Appiah-Opong, JN. Commandeur, B. van Vugt-Lussenburg, NP. Vermeulen, Inhibition of human recombinant cytochrome P450s by curcumin and curcumin decomposition products., Toxicology, volume 235, issue 1-2, pages 83-91, Jun 2007, doi [http://dx.doi.org/10.1016/j.tox.2007.03.007 10.1016/j.tox.2007.03.007], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17433521 17433521]</ref> | ||
| + | <ref name="Oetari-1996">S. Oetari, M. Sudibyo, JN. Commandeur, R. Samhoedi, NP. Vermeulen, Effects of curcumin on cytochrome P450 and glutathione S-transferase activities in rat liver., Biochem Pharmacol, volume 51, issue 1, pages 39-45, Jan 1996, PMID [http://www.ncbi.nlm.nih.gov/pubmed/8534266 8534266]</ref> | ||
| + | <ref name="Basu-2004">NK. Basu, M. Ciotti, MS. Hwang, L. Kole, PS. Mitra, JW. Cho, IS. Owens, Differential and special properties of the major human UGT1-encoded gastrointestinal UDP-glucuronosyltransferases enhance potential to control chemical uptake., J Biol Chem, volume 279, issue 2, pages 1429-41, Jan 2004, doi [http://dx.doi.org/10.1074/jbc.M306439200 10.1074/jbc.M306439200], PMID [http://www.ncbi.nlm.nih.gov/pubmed/14557274 14557274]</ref> | ||
| + | <ref name="Hayeshi-2007">R. Hayeshi, I. Mutingwende, W. Mavengere, V. Masiyanise, S. Mukanganyama, The inhibition of human glutathione S-transferases activity by plant polyphenolic compounds ellagic acid and curcumin., Food Chem Toxicol, volume 45, issue 2, pages 286-95, Feb 2007, doi [http://dx.doi.org/10.1016/j.fct.2006.07.027 10.1016/j.fct.2006.07.027], PMID [http://www.ncbi.nlm.nih.gov/pubmed/17046132 17046132]</ref> | ||
| + | <ref name="VareedKakarala2008">S. K. Vareed, M. Kakarala, M. T. Ruffin, J. A. Crowell, D. P. Normolle, Z. Djuric, D. E. Brenner, Pharmacokinetics of Curcumin Conjugate Metabolites in Healthy Human Subjects, Cancer Epidemiology Biomarkers & Prevention, volume 17, issue 6, 2008, pages 1411–1417, ISSN [http://www.worldcat.org/issn/1055-9965 1055-9965], doi [http://dx.doi.org/10.1158/1055-9965.EPI-07-2693 10.1158/1055-9965.EPI-07-2693]</ref> | ||
| + | <ref name="Burgos-MorónCalderón-Montaño2010">Estefanía Burgos-Morón, José Manuel Calderón-Montaño, Javier Salvador, Antonio Robles, Miguel López-Lázaro, The dark side of curcumin, International Journal of Cancer, 2010, pages NA–NA, ISSN [http://www.worldcat.org/issn/00207136 00207136], doi [http://dx.doi.org/10.1002/ijc.24967 10.1002/ijc.24967]</ref> | ||
| + | <ref name="BhutaniBishnoi2009">Mohit Kumar Bhutani, Mahendra Bishnoi, Shrinivas K. Kulkarni, Anti-depressant like effect of curcumin and its combination with piperine in unpredictable chronic stress-induced behavioral, biochemical and neurochemical changes, Pharmacology Biochemistry and Behavior, volume 92, issue 1, 2009, pages 39–43, ISSN [http://www.worldcat.org/issn/00913057 00913057], doi [http://dx.doi.org/10.1016/j.pbb.2008.10.007 10.1016/j.pbb.2008.10.007]</ref> | ||
| + | <ref name="Suresh-2010">D. Suresh, K. Srinivasan, Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats., Indian J Med Res, volume 131, pages 682-91, May 2010, PMID [http://www.ncbi.nlm.nih.gov/pubmed/20516541 20516541]</ref> | ||
| + | <ref name="Singh-1986">J. Singh, RK. Dubey, CK. Atal, Piperine-mediated inhibition of glucuronidation activity in isolated epithelial cells of the guinea-pig small intestine: evidence that piperine lowers the endogeneous UDP-glucuronic acid content., J Pharmacol Exp Ther, volume 236, issue 2, pages 488-93, Feb 1986, PMID [http://www.ncbi.nlm.nih.gov/pubmed/3080587 3080587]</ref> | ||
| + | <ref name="Shoba-1998">G. Shoba, D. Joy, T. Joseph, M. Majeed, R. Rajendran, PS. Srinivas, Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers., Planta Med, volume 64, issue 4, pages 353-6, May 1998, doi [http://dx.doi.org/10.1055/s-2006-957450 10.1055/s-2006-957450], PMID [http://www.ncbi.nlm.nih.gov/pubmed/9619120 9619120]</ref> | ||
| + | <ref name="Arcaro-2014">CA. Arcaro, VO. Gutierres, RP. Assis, TF. Moreira, PI. Costa, AM. Baviera, IL. Brunetti, Piperine, a natural bioenhancer, nullifies the antidiabetic and antioxidant activities of curcumin in streptozotocin-diabetic rats., PLoS One, volume 9, issue 12, pages e113993, 2014, doi [http://dx.doi.org/10.1371/journal.pone.0113993 10.1371/journal.pone.0113993], PMID [http://www.ncbi.nlm.nih.gov/pubmed/25469699 25469699]</ref> | ||
| + | <ref name="Garcea-2005">G. Garcea, DP. Berry, DJ. Jones, R. Singh, AR. Dennison, PB. Farmer, RA. Sharma, WP. Steward, AJ. Gescher, Consumption of the putative chemopreventive agent curcumin by cancer patients: assessment of curcumin levels in the colorectum and their pharmacodynamic consequences., Cancer Epidemiol Biomarkers Prev, volume 14, issue 1, pages 120-5, Jan 2005, PMID [http://www.ncbi.nlm.nih.gov/pubmed/15668484 15668484]</ref> | ||
| + | <ref name="AnandKunnumakkara2007">Preetha Anand, Ajaikumar B. Kunnumakkara, Robert A. Newman, Bharat B. Aggarwal, Bioavailability of Curcumin: Problems and Promises, Molecular Pharmaceutics, volume 4, issue 6, 2007, pages 807–818, ISSN [http://www.worldcat.org/issn/1543-8384 1543-8384], doi [http://dx.doi.org/10.1021/mp700113r 10.1021/mp700113r]</ref> | ||
| + | <ref name="TayyemHeath2006">Reema F. Tayyem, Dennis D. Heath, Wael K. Al-Delaimy, Cheryl L. Rock, Curcumin Content of Turmeric and Curry Powders, Nutrition and Cancer, volume 55, issue 2, 2006, pages 126–131, ISSN [http://www.worldcat.org/issn/0163-5581 0163-5581], doi [http://dx.doi.org/10.1207/s15327914nc5502_2 10.1207/s15327914nc5502_2]</ref> | ||
| + | <ref name="NiemanCialdella-Kam2012">David C. Nieman, Lynn Cialdella-Kam, Amy M. Knab, R. Andrew Shanely, Influence of Red Pepper Spice and Turmeric on Inflammation and Oxidative Stress Biomarkers in Overweight Females: A Metabolomics Approach, Plant Foods for Human Nutrition, volume 67, issue 4, 2012, pages 415–421, ISSN [http://www.worldcat.org/issn/0921-9668 0921-9668], doi [http://dx.doi.org/10.1007/s11130-012-0325-x 10.1007/s11130-012-0325-x]</ref> | ||
| + | <ref name="CarrollDickinson2011">C. C. Carroll, J. M. Dickinson, J. K. LeMoine, J. M. Haus, E. M. Weinheimer, C. J. Hollon, P. Aagaard, S. P. Magnusson, T. A. Trappe, Influence of acetaminophen and ibuprofen on in vivo patellar tendon adaptations to knee extensor resistance exercise in older adults, Journal of Applied Physiology, volume 111, issue 2, 2011, pages 508–515, ISSN [http://www.worldcat.org/issn/8750-7587 8750-7587], doi [http://dx.doi.org/10.1152/japplphysiol.01348.2010 10.1152/japplphysiol.01348.2010]</ref> | ||
</references> | </references> | ||
| + | [[Category:Training]] | ||
| + | [[Category:Injury]] | ||
| + | [[Category:Science]] | ||
Latest revision as of 13:40, 22 December 2016
NSAIDs are generally unhelpful for runners, masking the symptoms while impairing healing, interfering with hydration and can be life threatening. Risks include kidney failure, heart attacks, strokes, intestinal damage, and liver failure. The most common NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are Ibuprofen (Advil, Motrin), Naproxen (Aleve, Naprosyn), and Aspirin. They work by inhibiting a particular enzyme (Cyclooxygenase) which reduces pain, fever and inflammation. Ibuprofen use is so common among runners that it is sometimes called "Vitamin I"[1], with one study finding about 60% of runners using NSAIDs during training[2]. This is unsurprising given the estimates of injury rates in runners varying between 20% and 80%[3]. This article also covers Acetaminophen (also called Paracetamol), though it's not technically an NSAID.
Contents
[hide]- 1 NSAIDs and Healing
- 2 Turmeric as an NSAID
- 3 NSAIDs and Acute kidney failure
- 4 NSAIDs and Hyponatremia
- 5 NSAIDs causing Heart Attacks or Strokes
- 6 NSAIDs and Infection
- 7 NSAIDs for Pain Reduction
- 8 NSAIDs and DOMS
- 9 NSAIDs and Intestinal Damage
- 10 NSAIDs and Wound Healing
- 11 NSAIDs and Racing
- 12 Longer Term NSAID usage
- 13 Acetaminophen Overdose Danger (AKA Paracetamol, Tylenol)
- 14 Is Acetaminophen an NSAID?
- 15 References
1 NSAIDs and Healing
The inflammation response of our bodies is a key part of the healing process. Using NSAIDs to reduce the inflammation has been shown to impair healing in different tissue types:
- Muscles[4]. A 2001 study showed that Ibuprofen and Acetaminophen reduce muscle growth after eccentric exercise. Another study[5] on muscle damage and NSAIDs showed impaired recovery in the early stages of healing. There was some increased Protein synthesis with NSAIDs in latter stages of healing, but the muscles were still weaker 28 days after injury. Other studies[6][7] have shown that four days after injury, NSAIDs resulted in very little muscle regeneration compared with no drugs.
- Tendons. A primate study[8] showed "a marked decrease in the breaking strength of tendons at four and six weeks in the ibuprofen-treated animals". Another animal study[9] showed treated tendons were 32% weaker than their untested counterparts. A study of older adults showed a weakening of tendons with acetaminophen (but not ibuprofen) use[10].
- Bone-Tendon Junctions. An animal study[11] of rotator cuff injuries shows that NSAID usage resulted in injuries that did not heal, and those that did heal were weaker than those without NSAID. To quote from the study "Given that NSAID administration was discontinued after 14 days yet affected load-to-failure eight weeks following repair, it appears that inhibition of the early events in the inflammatory cascade has a lasting negative effect on tendon-to-bone healing," Dr. Rodeo said.
- Cartilage. NSAIDs have been shown[12] to impair the healing of bone and cartilage in rabbits.
- Bone fractures. Tests on rats shows that a NSAID (Celecoxib) in the early stages of bone healing impaired healing, producing a weaker repair.[13] A study [14] in 2004 declared " Nonsteroidal anti-inflammatory drugs continue to be prescribed as analgesics for patients with healing fractures even though these drugs diminish bone formation, healing, and remodeling".
1.1 Counterpoint
While there is extensive experimental evidence for NSAIDs impairing healing, there are also some studies that show no change with NSAID use, and a few that indicated improved healing. For instance, one study[15] showed that using an NSAID for 6 days after injury resulted in a 42% increased ligament strength at day 14, though there was no change by day 21. Another study[16] showed that an NSAID did not change ligament healing, but did improve the strength of the uninjured ligaments. However, my reading indicates that the preponderance of evidence shows NSAIDs impair healing.
1.2 Ice, Inflammation and Healing
If NSAIDs are bad for healing, should we treat with ice? So far I have found no definitive studies, but ice has a different mechanism of action from NSAIDs. By cooling the tissues, ice temporarily reduces swelling, thereby flushing the wound. If applied for a longer period of time, ice will produce a periodic increase in blood supply that creates a further flushing effect. I have found that ice can produce dramatic improvements in healing speed. See Cryotherapy - Ice for Healing for more details. There is no evidence that ice reduces any of the inflammation processes.
2 Turmeric as an NSAID
Turmeric is an anti-inflammatory[17][18] that is often considered an alternative to more common NSAIDs. Like other NSAIDs, Turmeric is an effective pain reliever (analgesic)[19][20][21][22] and it may be effective in treating Delayed Onset Muscle Soreness[23][24][25][26][27][28]. Studies of Turmeric and turmeric derivatives as treatments for osteoarthritis[29][30], rheumatoid arthritis[31], and cancer[32][33][34] show potentially promising results. However, there are concerns that most of the human studies on Turmeric are of poor quality and should be treated with caution[35].
2.1 Turmeric Safety
Turmeric has been medicinally used for 1000s of years[36] and even in large doses turmeric shows low acute toxicity[37][32][31][38] with only a few studies finding nausea and diarrhea[37] or abdominal pain[30]. However, there are concerns that many studies on Turmeric are in vitro (isolated tissues) at dose levels that are hard to replicate in humans[39]. Doses as high as 12g of curcumin produce negligible levels in the blood[40]. At therapeutic levels there is evidence that Turmeric (curcumin) may be carcinogenic[41][42][43][44][45][46][47][48][49], though it can exhibit both anticancer and carcinogenic properties[50]. Curcumin can inhibit liver function, including the drug-metabolizing P450 enzymes[51][52][53][54][55]. (This could cause problematic drug interactions.) Turmeric may bind to iron, resulting in iron deficiency[56][57], though it has been suggested that some of the benefits of Turmeric are from this iron binding[58]. It should be remembered that other common constituents of normal diet have shown to be toxic when used as dietary supplements[59]
2.2 Turmeric Doses
It's been estimated people in India consuming high culinary intakes of Turmeric obtain about 150mg/day of curcumin[60], and average intake is probably 60-100mg/day[61]. However, must studies use much higher levels, and culinary levels (~2g/day) Turmeric is probably ineffective as an NSAID[62]. Turmeric has poor bioavailability[63][64] due to poor absorption and rapid metabolism[64]. The curcumin level in Turmeric powder can vary dramatically, with one study finding levels between 0.6 and 3.1% dry weight, a more than five-fold variation[65]. This makes it hard to use the raw powder, as the actual dose could vary enormously and a high dose of curcumin such as 8g would potentially require the consumption of 1.3Kg/2.8 pounds of Turmeric powder. It's been shown that 3.6 g curcumin produces effective levels in the digestive system, but negligible levels outside the gut[66], and even 12g of curcumin produce negligible levels in the blood[40]. This is compounded by the rapid removal, with concentrations of curcumin typically peak 1-2 hours after consumption and declining within 12 hours[32][19]. At this point, it's hard to define a dose of Turmeric or curcumin beyond saying that it's safe at culinary levels (~2g/day of Turmeric powder).
2.3 Turmeric Enhancers
The levels of Turmeric can be enhanced by taking it with piperine, a constituent of black pepper. One study that gave subjects 2g of curcumin found extremely low levels in the blood, but adding 20mg of piperine boosted blood levels by 2000%[67]. Another animal study using intravenous administration found piperine enhanced the effectiveness of curcumin[68]. However, an animal study found that low levels (20 mg/kg) of piperine did not enhance the effectiveness of curcumin, and higher levels (40 mg/kg) actually negated the curcumin benefits[69]. Piperine increases the absorption of curcumin[70] and reduces the metabolism of curcumin by the liver[67][55]. However, the reduced metabolism is because like curcumin, piperine is a powerful inhibitor of liver function[71][72][73]. Personally, I am cautious about boosting the levels of curcumin by impairing the liver. There are also versions of curcumin with improved bioavailability are being developed such as Flexofytol[74] or Meriva[24]. However, it should be noted that the bulk of the current research does not use enhancers, so caution may be appropriate.
2.4 Turmeric as a selective COX-2 Inhibitor
Digestive problems, a common side effect of NSAIDs, are believed to be because most NSAIDs inhibit both COX-1 and COX-2 enzymes[75]. COX-2 is predominantly responsible for inflammation where COX-1 helps maintain the digestive system[76]. Selectively inhibiting just COX-2 may have the benefits of NSAIDS without the digestive issues[77][78][76]. Studies have found that Turmeric is a COX-2 inhibitor[79][80][81][82][83], and turmeric preferentially inhibits COX-2 over COX-1[84]. Turmeric has ~36% COX-1 inhibition and ~77% COX-2 inhibition, while aspirin, ibuprofen and naproxen had 41-52% COX-1 inhibition and ~30-40% COX-2 inhibition[84]. Diferuloylmethane (Curcumin) is the main active ingredient in turmeric[63][85], though it also includes monodemethoxycurcumin (curcumin II) and bisdemethoxycurcumin (curcumin III)[84].
3 NSAIDs and Acute kidney failure
Kidney failure while running is extremely rare, and seems to require multiple factors to come together. Looking at the Comrades Marathon, a 90 Km/56 Mile ultramarathon in South Africa, there have only been 19 cases of kidney failure between 1969 and 1986, it even though thousands of people participate each year[86]. The following are considered factors in acute kidney failure related to running.
- Dehydration. Exercise reduces blood flow to the kidneys and dehydration makes this worse.
- NSAIDs. NSAIDs also reduce blood flow to the kidneys[87]. NSAIDs reduce prostaglandin production, and prostaglandins are vital to maintaining blood flow to the kidneys. While NSAIDs are considered safe drugs, NSAIDs are associated with a relatively high incidence of adverse drug reactions involving the kidneys. Generally, NSAID side effects are restricted to individuals with predisposition to kidney problems, so extra care should be taken if you have a history of kidney problems. However, athletes push their bodies to extremes, so what applies to the general population may not be valid for runners. One runner was told[88] by doctors that 2400mg Ibuprofen in an ultramarathon was a contributing factor to his kidney failure.
- Rhabdomyolysis. All strenuous exercise causes some muscle damage, but this is generally resolved without a problem. However large amounts of a Protein called myoglobin from damaged muscle can cause a condition called rhabdomyolysis (AKA 'rhabdo'). While serious rhabdomyolysis is rare, it is worth understanding one key symptom, which is low volume, dark urine, often likened to 'coca-cola'. The other symptoms include severe, incapacitating muscle pain and elevated levels of creatine kinase (CK) in the blood (which requires a specialist test). Some individuals[89] have a genetic condition that makes rhabdomyolysis possible after relatively moderate exercise. Rhabdomyolysis is also more likely after eccentric exercise, such as Downhill Running.
- Sickness. A viral or bacterial infection is often a factor in exercise related kidney failure.
Looking at the analysis[87] of nine cases of continued kidney failure in Comrades Marathon, seven had taken NSAIDs, four may have had a viral or bacterial infection. The combination of dehydration, rhabdomyolysis, infection and NSAIDs are a perfect storm for the kidneys.
4 NSAIDs and Hyponatremia
The kidneys are responsible for removing excess fluid from the blood as well as excreting or withholding sodium. If kidney function is compromised, then this can result in Hyponatremia, which can be fatal. Some studies[90][91][92] have shown a correlation between NSAID use in races and Hyponatremia, but others[93][94] have not. Using NSAIDs when hydration is a concern increases the risk of problems occuring.
5 NSAIDs causing Heart Attacks or Strokes
The U.S. Food and Drug Administration (FDA) warnings that non-aspirin NSAIDs increase the risk of a heart attack or stroke[95]. The risk appears to be related to ongoing usage rather than single doses, with the risk increasing in the first weeks of usage and the risk may increase with prolonged usage. The increased risk is dose dependent (taking more has a greater risk), and the includes those without heart disease or risk factors for heart disease. Not surprisingly, those already with a higher risk of heart disease or stroke have a proportionately higher risk with NSAID usage.
6 NSAIDs and Infection
Because a bacterial or viral infection puts more stress on the body, including the kidneys, taking NSAIDs and continuing to run increases your risk of complications. If the sickness is too bad to run without NSAIDs, you probably shouldn't run.
7 NSAIDs for Pain Reduction
The primary purpose of NSAIDs is generally for reducing pain, and they are remarkably effective at achieving this. If you need a painkiller, acetaminophen is probably a better choice than ibuprofen, though be careful as it's easy to overdose on Acetaminophen (see below). Acetaminophen has limited anti-inflammatory properties, so it shouldn't impair healing as much as ibuprofen, but it is still good as a painkiller. Combining acetaminophen or other NSAIDs with Caffeine further improves their painkilling effectiveness. After a major race I can sometimes have so much leg pain that I can't sleep and a little acetaminophen can make all the difference. While the acetaminophen may impair healing somewhat I believe the trade-off in improved sleep is worthwhile. After all, the lack of sleep itself will impair healing, so it's a reasonable compromise.
8 NSAIDs and DOMS
Main article: Delayed Onset Muscle Soreness
Delayed Onset Muscle Soreness (DOMS) generally occurs between 24 and 72 hours after unusual or severe exercise, such as racing a marathon or Downhill Running. The use of NSAIDs to prevent or treat DOMS has been widely researched, with somewhat mixed results. Even scholarly reviews of the research have differing conclusions[96] [97] [98][99]. My conclusions based on the available research are:
- The most common NSAIDs (Ibuprofen, Acetaminophen (Paracetamol), and Aspirin) are unlikely to help with DOMS.
- There is some evidence that Naproxen may be more effective than the common NSAIDs. There is not enough evidence to reach a conclusion on Diclofenac, Codeine, Rofecoxib, Ketoprofen, or Bromelain.
- There is also some evidence that Turmeric may help with DOMS.
- If an NSAID is taken for DOMS, it should probably be taken immediately after the damaging exercise rather than waiting until the soreness develops.
- It seems likely that taking an NSAID for DOMS will reduce the muscular growth that would normally occur as part of the recovery. In one study, rabbits treated with flurbiprofen after DOMS inducing exercise regained more strength after 3-7 days, but between days 7 and 28 days the treated rabbits became weaker while the controls became stronger[100]. This is only one study, and on animals, but it is rather troubling as none of the human studies look at the results over this time period.
8.1 A Summary of the Research on NSAIDs and DOMS
The table below summarizes the research I located on the effect of NSAIDs on DOMS in humans. I've only considered the primary DOMS markers of soreness (pain) and weakness, rather than including things like blood enzymes. For each NSAID I've shown how many studies show an improvement and how many studies show no effect.
| NSAID | Soreness | Weakness |
|---|---|---|
| Ibuprofen | 2xImproved[101][102] | 1xMaybe[101] |
| Ibuprofen Gel | 1xNo Effect[110] | |
| Acetaminophen (Paracetamol) | 2xNo Effect[111][112] | |
| Aspirin | 2xImproved[113][114] | 2xNo Effect[113][114] |
| Naproxen | 4xImproved[115][116][117][118]
1xNo Effect[119] |
3xImproved[115][116][117]
1xNo Effect[119] |
| Diclofenac | Possible slight reduction[120] | |
| Codeine | 1xNo Effect[111] | |
| Rofecoxib | 1xNo Effect[121] | |
| Ketoprofen | 1xImproved[122] | 1xImproved[122] |
| Bromelain | 1xNo Effect[109] | |
| Turmeric | 2xImproved[23][24] | 2xImproved[26][27] |
9 NSAIDs and Intestinal Damage
As little as one hour of intense cycling can result in indications of small intestinal damage[123]. This is believed to be due to the redirection of blood away from the digestive system and towards the active muscles. These markers are significantly higher if 400mg ibuprofen (the standard single adult dose) is taken before the exercise[124]. The marker used is Plasma Intestinal Fatty Acid Binding Protein which is an early marker of intestinal necrosis[125].
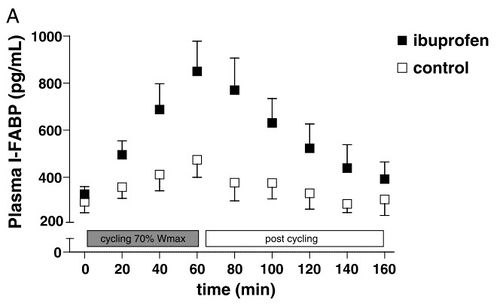
10 NSAIDs and Wound Healing
Main article: Popping Blisters
Ibuprofen, and possibly other NSAIDs, impair wound healing and should be avoided[126][127].
11 NSAIDs and Racing
Taking NSAIDs in ultramarathon events can improve performance by reducing pain and acute inflammation, but doing so represents a significant risk. There is some evidence[128] [129] that many runners taking NSAIDs have the same level of pain and greater damage markers compared with non-users. This may be because the runners push themselves to a similar level of pain, with the NSAIDs allowing them to do more damage.
- It seems likely that NSAIDs will increase the risk of injury rather than reducing it, as the symptoms of damage will be masked.
- The most common NSAID for racing seems to be ibuprofen. I've not seen any evidence of the relative effectiveness of different NSAIDs on performance.
- It is better to take liquid ibuprofen than tablets or capsules. The tablets and capsules take longer to dissolve and if you have a digestive problem they may not be fully absorbed. You can chew the tablets, but this is unpleasant and ibuprofen can irritate your mouth and throat slightly, so the liquid form is best. It's obviously harder to transport, but you can fill an old film canister with a dose.
- Before an ultramarathon race, you should think through under what circumstances you will consider using NSAIDs and what dosage. Make sure your crew knows that you're taking NSAIDs in case anything happens.
- Extra care should be taken when NSAIDs are used in combination with dehydration, sickness or running the causes serious muscle damage.
- Taking NSAIDs in marathon or shorter races is probably ineffective as the level of damage seen is not as great as in ultramarathon events.
- If you need NSAIDs to start a race, you probably should not compete.
12 Longer Term NSAID usage
Using NSAIDs for longer periods of time can lead to serious health problems and can be fatal. I have a running friend who had a bleeding ulcer from using Ibuprofen, which is a known[130] side effect. The likelihood of a bleeding or perforated ulcer goes up with time, from 1% after 3-6 months, to 2-4% after 12 months. 35% of long term Ibuprofen users get an ulcer[131], which are grim odds.
13 Acetaminophen Overdose Danger (AKA Paracetamol, Tylenol)
Acetaminophen does not have the same risk of ulcers, but it is linked to liver damage, especially in those who drink alcohol. Acetaminophen is the leading cause of acute liver failure[132][133]. There are concerns[134] that even the standard dose can cause changes in liver function. Acetaminophen can cause delayed symptoms[133], with people seeking medical help up to 5 days after the overdose (20% < 12 hours, 35% 12-24 hours, 45% 24 hours+). Overdoses of Acetaminophen can be caused by taking slightly too much over several days, with the toxicity building up[133]. This problem is again exacerbated by those taking alcohol with Acetaminophen[133]. (One factor that increases the risk is that some common medications, such as cold remedies, include Acetaminophen. If people do not add in the dose of Acetaminophen from these other sources, it is easy to unwittingly exceed the safe dosage.)
14 Is Acetaminophen an NSAID?
Acetaminophen (also called paracetamol) is generally not classified as an NSAID[135]. While Acetaminophen has limited anti-inflammatory properties, it shares the same mechanism of action with most NSAIDs of inhibiting the COX enzyme and the inhibition of prostaglandin synthesis[136][137][138][139]. Therefore, this article includes Acetaminophen in with NSAIDs.
15 References
- Jump up ↑ Urban Dictionary: Vitamin I http://www.urbandictionary.com/define.php?term=Vitamin%20I
- Jump up ↑ Jeremy D Joslin, Jarem B Lloyd, Timur Kotlyar, Susan M Wojcik, NSAID and other analgesic use by endurance runners during training, competition and recovery, South African Journal of Sports Medicine, volume 25, issue 4, 2013, pages 101, ISSN 2078-516X, doi 10.7196/sajsm.495
- Jump up ↑ RN. van Gent, D. Siem, M. van Middelkoop, AG. van Os, SM. Bierma-Zeinstra, BW. Koes, Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review., Br J Sports Med, volume 41, issue 8, pages 469-80; discussion 480, Aug 2007, doi 10.1136/bjsm.2006.033548, PMID 17473005
- Jump up ↑ Skeletal Muscle PGF2αand PGE2 in Response to Eccentric Resistance Exercise: Influence of Ibuprofen and Acetaminophen http://jcem.endojournals.org/content/86/10/5067.long
- Jump up ↑ An In Vitro Investigation Into the Effects of Repetitive Motion and Nonsteroidal Antiinflammatory Medication on Human Tendon Fibroblasts http://ajs.sagepub.com/content/23/1/119
- Jump up ↑ Cost-conscious prescribing of nonsteroidal anti-in... [Arch Intern Med. 1992] - PubMed result http://www.ncbi.nlm.nih.gov/pubmed/1417372
- Jump up ↑ Sports Injuries - NSAIDs: Why We Do Not Recommend Them http://www.caringmedical.com/sports_injury/nsaids.asp
- Jump up ↑ Oral ibuprofen: evaluation of its effect on peritendinous adhesions and the breaking strength of a tenorrhaphy. [J Hand Surg Am. 1986] - PubMed result http://www.ncbi.nlm.nih.gov/pubmed/3511134#
- Jump up ↑ A cyclooxygenase-2 inhibitor impairs ligament heal... [Am J Sports Med. 2001 Nov-Dec] - PubMed result http://www.ncbi.nlm.nih.gov/pubmed/11734496?dopt=Abstract&holding=npg
- Jump up ↑ C. C. Carroll, J. M. Dickinson, J. K. LeMoine, J. M. Haus, E. M. Weinheimer, C. J. Hollon, P. Aagaard, S. P. Magnusson, T. A. Trappe, Influence of acetaminophen and ibuprofen on in vivo patellar tendon adaptations to knee extensor resistance exercise in older adults, Journal of Applied Physiology, volume 111, issue 2, 2011, pages 508–515, ISSN 8750-7587, doi 10.1152/japplphysiol.01348.2010
- Jump up ↑ NSAIDs Inhibit Tendon-to-Bone Healing in Rotator Cuff Repair http://www.shoulderdoc.co.uk/article.asp?article=295
- Jump up ↑ Effect of ibuprofen on the healing and remodeling of bone and articular cartilage in the rabbit temporomandibular joint http://www.joms.org/article/0278-2391%2892%2990276-6/abstract
- Jump up ↑ JBJS | Dose and Time-Dependent Effects of Cyclooxygenase-2 Inhibition on Fracture-Healing http://www.jbjs.org/article.aspx?Volume=89&page=500
- Jump up ↑ Effects of Nonsteroidal Anti-Inflammatory Drugs on Bone Formation and Soft-Tissue Healing -- Dahners and Mullis 12 (3): 139 -- Journal of the American Academy of Orthopaedic Surgeons http://www.jaaos.org/cgi/content/abstract/12/3/139
- Jump up ↑ The effect of a nonsteroidal antiinflammatory drug... [Am J Sports Med. 1988 Nov-Dec] - PubMed result http://www.ncbi.nlm.nih.gov/pubmed/3239621?dopt=Abstract&holding=npg
- Jump up ↑ The influence of a cyclooxygenase-1 inhibitor on i... [Am J Sports Med. 2003 Jul-Aug] - PubMed result http://www.ncbi.nlm.nih.gov/pubmed/12860547
- Jump up ↑ Amirhossein Sahebkar, Are Curcuminoids Effective C-Reactive Protein-Lowering Agents in Clinical Practice? Evidence from a Meta-Analysis, Phytotherapy Research, volume 28, issue 5, 2014, pages 633–642, ISSN 0951418X, doi 10.1002/ptr.5045
- Jump up ↑ Y. Panahi, A. Sahebkar, S. Parvin, A. Saadat, A randomized controlled trial on the anti-inflammatory effects of curcumin in patients with chronic sulphur mustard-induced cutaneous complications, Annals of Clinical Biochemistry, volume 49, issue 6, 2012, pages 580–588, ISSN 0004-5632, doi 10.1258/acb.2012.012040
- ↑ Jump up to: 19.0 19.1 KA. Agarwal, CD. Tripathi, BB. Agarwal, S. Saluja, Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study., Surg Endosc, volume 25, issue 12, pages 3805-10, Dec 2011, doi 10.1007/s00464-011-1793-z, PMID 21671126
- Jump up ↑ Y. Panahi, AR. Rahimnia, M. Sharafi, G. Alishiri, A. Saburi, A. Sahebkar, Curcuminoid treatment for knee osteoarthritis: a randomized double-blind placebo-controlled trial., Phytother Res, volume 28, issue 11, pages 1625-31, Nov 2014, doi 10.1002/ptr.5174, PMID 24853120
- Jump up ↑ V. Kuptniratsaikul, S. Thanakhumtorn, P. Chinswangwatanakul, L. Wattanamongkonsil, V. Thamlikitkul, Efficacy and safety of Curcuma domestica extracts in patients with knee osteoarthritis., J Altern Complement Med, volume 15, issue 8, pages 891-7, Aug 2009, doi 10.1089/acm.2008.0186, PMID 19678780
- Jump up ↑ X. Zhu, Q. Li, R. Chang, D. Yang, Z. Song, Q. Guo, C. Huang, Curcumin alleviates neuropathic pain by inhibiting p300/CBP histone acetyltransferase activity-regulated expression of BDNF and cox-2 in a rat model., PLoS One, volume 9, issue 3, pages e91303, 2014, doi 10.1371/journal.pone.0091303, PMID 24603592
- ↑ Jump up to: 23.0 23.1 LM. Nicol, DS. Rowlands, R. Fazakerly, J. Kellett, Curcumin supplementation likely attenuates delayed onset muscle soreness (DOMS)., Eur J Appl Physiol, volume 115, issue 8, pages 1769-77, Aug 2015, doi 10.1007/s00421-015-3152-6, PMID 25795285
- ↑ Jump up to: 24.0 24.1 24.2 F. Drobnic, J. Riera, G. Appendino, S. Togni, F. Franceschi, X. Valle, A. Pons, J. Tur, Reduction of delayed onset muscle soreness by a novel curcumin delivery system (Meriva): a randomised, placebo-controlled trial., J Int Soc Sports Nutr, volume 11, pages 31, 2014, doi 10.1186/1550-2783-11-31, PMID 24982601
- ↑ Jump up to: 25.0 25.1 Brian K. McFarlin, Adam S. Venable, Andrea L. Henning, Jill N. Best Sampson, Kathryn Pennel, Jakob L. Vingren, David W. Hill, Reduced Inflammatory and Muscle Damage Biomarkers following Oral Supplementation with Bioavailable Curcumin, BBA Clinical, 2016, ISSN 22146474, doi 10.1016/j.bbacli.2016.02.003
- ↑ Jump up to: 26.0 26.1 26.2 Yoko Tanabe, Seiji Maeda, Nobuhiko Akazawa, Asako Zempo-Miyaki, Youngju Choi, Song-Gyu Ra, Atsushi Imaizumi, Yoshihiko Otsuka, Kazunori Nosaka, Attenuation of indirect markers of eccentric exercise-induced muscle damage by curcumin, European Journal of Applied Physiology, volume 115, issue 9, 2015, pages 1949–1957, ISSN 1439-6319, doi 10.1007/s00421-015-3170-4
- ↑ Jump up to: 27.0 27.1 JM. Davis, EA. Murphy, MD. Carmichael, MR. Zielinski, CM. Groschwitz, AS. Brown, JD. Gangemi, A. Ghaffar, EP. Mayer, Curcumin effects on inflammation and performance recovery following eccentric exercise-induced muscle damage., Am J Physiol Regul Integr Comp Physiol, volume 292, issue 6, pages R2168-73, Jun 2007, doi 10.1152/ajpregu.00858.2006, PMID 17332159
- Jump up ↑ N. Kawanishi, K. Kato, M. Takahashi, T. Mizokami, Y. Otsuka, A. Imaizumi, D. Shiva, H. Yano, K. Suzuki, Curcumin attenuates oxidative stress following downhill running-induced muscle damage., Biochem Biophys Res Commun, volume 441, issue 3, pages 573-8, Nov 2013, doi 10.1016/j.bbrc.2013.10.119, PMID 24184481
- Jump up ↑ Y. Henrotin, M. Gharbi, Y. Dierckxsens, F. Priem, M. Marty, L. Seidel, A. Albert, E. Heuse, V. Bonnet, Decrease of a specific biomarker of collagen degradation in osteoarthritis, Coll2-1, by treatment with highly bioavailable curcumin during an exploratory clinical trial., BMC Complement Altern Med, volume 14, pages 159, 2014, doi 10.1186/1472-6882-14-159, PMID 24886572
- ↑ Jump up to: 30.0 30.1 V. Kuptniratsaikul, P. Dajpratham, W. Taechaarpornkul, M. Buntragulpoontawee, P. Lukkanapichonchut, C. Chootip, J. Saengsuwan, K. Tantayakom, S. Laongpech, Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: a multicenter study., Clin Interv Aging, volume 9, pages 451-8, 2014, doi 10.2147/CIA.S58535, PMID 24672232
- ↑ Jump up to: 31.0 31.1 B. Chandran, A. Goel, A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis., Phytother Res, volume 26, issue 11, pages 1719-25, Nov 2012, doi 10.1002/ptr.4639, PMID 22407780
- ↑ Jump up to: 32.0 32.1 32.2 AL. Cheng, CH. Hsu, JK. Lin, MM. Hsu, YF. Ho, TS. Shen, JY. Ko, JT. Lin, BR. Lin, Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions., Anticancer Res, volume 21, issue 4B, pages 2895-900, PMID 11712783
- Jump up ↑ S. Rao, C. Dinkar, L. K. Vaishnav, P. Rao, M. P. Rai, R. Fayad, M. S. Baliga, The Indian Spice Turmeric Delays and Mitigates Radiation-Induced Oral Mucositis in Patients Undergoing Treatment for Head and Neck Cancer: An Investigational Study, Integrative Cancer Therapies, volume 13, issue 3, 2013, pages 201–210, ISSN 1534-7354, doi 10.1177/1534735413503549
- Jump up ↑ SC. Gupta, S. Patchva, BB. Aggarwal, Therapeutic roles of curcumin: lessons learned from clinical trials., AAPS J, volume 15, issue 1, pages 195-218, Jan 2013, doi 10.1208/s12248-012-9432-8, PMID 23143785
- Jump up ↑ C. Mancuso, E. Barone, Curcumin in clinical practice: myth or reality?, Trends Pharmacol Sci, volume 30, issue 7, pages 333-4, Jul 2009, doi 10.1016/j.tips.2009.04.004, PMID 19523696
- Jump up ↑ IFF. Benzie, S. Wachtel-Galor, S. Prasad, BB. Aggarwal, Turmeric, the Golden Spice: From Traditional Medicine to Modern Medicine, PMID 22593922
- ↑ Jump up to: 37.0 37.1 CH. Hsu, AL. Cheng, Clinical studies with curcumin., Adv Exp Med Biol, volume 595, pages 471-80, 2007, doi 10.1007/978-0-387-46401-5_21, PMID 17569225
- Jump up ↑ S. Ganiger, H.N. Malleshappa, H. Krishnappa, Geetha Rajashekhar, V. Ramakrishna Rao, Frank Sullivan, A two generation reproductive toxicity study with curcumin, turmeric yellow, in Wistar rats, Food and Chemical Toxicology, volume 45, issue 1, 2007, pages 64–69, ISSN 02786915, doi 10.1016/j.fct.2006.07.016
- Jump up ↑ Estefanía Burgos-Morón, José Manuel Calderón-Montaño, Javier Salvador, Antonio Robles, Miguel López-Lázaro, The dark side of curcumin, International Journal of Cancer, 2010, pages NA–NA, ISSN 00207136, doi 10.1002/ijc.24967
- ↑ Jump up to: 40.0 40.1 S. K. Vareed, M. Kakarala, M. T. Ruffin, J. A. Crowell, D. P. Normolle, Z. Djuric, D. E. Brenner, Pharmacokinetics of Curcumin Conjugate Metabolites in Healthy Human Subjects, Cancer Epidemiology Biomarkers & Prevention, volume 17, issue 6, 2008, pages 1411–1417, ISSN 1055-9965, doi 10.1158/1055-9965.EPI-07-2693
- Jump up ↑ C.E. Goodpasture, F.E. Arrighi, Effects of food seasonings on the cell cycle and chromosome morphology of mammalian cells in vitro with special reference to turmeric, Food and Cosmetics Toxicology, volume 14, issue 1, 1976, pages 9–14, ISSN 00156264, doi 10.1016/S0015-6264(76)80356-2
- Jump up ↑ AK. Giri, SK. Das, G. Talukder, A. Sharma, Sister chromatid exchange and chromosome aberrations induced by curcumin and tartrazine on mammalian cells in vivo., Cytobios, volume 62, issue 249, pages 111-7, 1990, PMID 2209081
- Jump up ↑ H. Ahsan, SM. Hadi, Strand scission in DNA induced by curcumin in the presence of Cu(II)., Cancer Lett, volume 124, issue 1, pages 23-30, Feb 1998, PMID 9500187
- Jump up ↑ K. Sakano, S. Kawanishi, Metal-mediated DNA damage induced by curcumin in the presence of human cytochrome P450 isozymes., Arch Biochem Biophys, volume 405, issue 2, pages 223-30, Sep 2002, PMID 12220536
- Jump up ↑ J. Nair, S. Strand, N. Frank, J. Knauft, H. Wesch, PR. Galle, H. Bartsch, Apoptosis and age-dependant induction of nuclear and mitochondrial etheno-DNA adducts in Long-Evans Cinnamon (LEC) rats: enhanced DNA damage by dietary curcumin upon copper accumulation., Carcinogenesis, volume 26, issue 7, pages 1307-15, Jul 2005, doi 10.1093/carcin/bgi073, PMID 15790590
- Jump up ↑ J. Blasiak, A. Trzeciak, J. Kowalik, Curcumin damages DNA in human gastric mucosa cells and lymphocytes., J Environ Pathol Toxicol Oncol, volume 18, issue 4, pages 271-6, 1999, PMID 15281237
- Jump up ↑ MR. Kelly, J. Xu, KE. Alexander, G. Loo, Disparate effects of similar phenolic phytochemicals as inhibitors of oxidative damage to cellular DNA., Mutat Res, volume 485, issue 4, pages 309-18, May 2001, PMID 11585363
- Jump up ↑ J. Cao, L. Jia, HM. Zhou, Y. Liu, LF. Zhong, Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells., Toxicol Sci, volume 91, issue 2, pages 476-83, Jun 2006, doi 10.1093/toxsci/kfj153, PMID 16537656
- Jump up ↑ P. Urbina-Cano, L. Bobadilla-Morales, MA. Ramírez-Herrera, JR. Corona-Rivera, ML. Mendoza-Magaña, R. Troyo-Sanromán, A. Corona-Rivera, DNA damage in mouse lymphocytes exposed to curcumin and copper., J Appl Genet, volume 47, issue 4, pages 377-82, 2006, doi 10.1007/BF03194648, PMID 17132903
- Jump up ↑ M. López-Lázaro, Anticancer and carcinogenic properties of curcumin: considerations for its clinical development as a cancer chemopreventive and chemotherapeutic agent., Mol Nutr Food Res, volume 52 Suppl 1, pages S103-27, Jun 2008, doi 10.1002/mnfr.200700238, PMID 18496811
- Jump up ↑ R. Hayeshi, I. Mutingwende, W. Mavengere, V. Masiyanise, S. Mukanganyama, The inhibition of human glutathione S-transferases activity by plant polyphenolic compounds ellagic acid and curcumin., Food Chem Toxicol, volume 45, issue 2, pages 286-95, Feb 2007, doi 10.1016/j.fct.2006.07.027, PMID 17046132
- Jump up ↑ NK. Basu, M. Ciotti, MS. Hwang, L. Kole, PS. Mitra, JW. Cho, IS. Owens, Differential and special properties of the major human UGT1-encoded gastrointestinal UDP-glucuronosyltransferases enhance potential to control chemical uptake., J Biol Chem, volume 279, issue 2, pages 1429-41, Jan 2004, doi 10.1074/jbc.M306439200, PMID 14557274
- Jump up ↑ S. Oetari, M. Sudibyo, JN. Commandeur, R. Samhoedi, NP. Vermeulen, Effects of curcumin on cytochrome P450 and glutathione S-transferase activities in rat liver., Biochem Pharmacol, volume 51, issue 1, pages 39-45, Jan 1996, PMID 8534266
- Jump up ↑ R. Appiah-Opong, JN. Commandeur, B. van Vugt-Lussenburg, NP. Vermeulen, Inhibition of human recombinant cytochrome P450s by curcumin and curcumin decomposition products., Toxicology, volume 235, issue 1-2, pages 83-91, Jun 2007, doi 10.1016/j.tox.2007.03.007, PMID 17433521
- ↑ Jump up to: 55.0 55.1 LP. Volak, S. Ghirmai, JR. Cashman, MH. Court, Curcuminoids inhibit multiple human cytochromes P450, UDP-glucuronosyltransferase, and sulfotransferase enzymes, whereas piperine is a relatively selective CYP3A4 inhibitor., Drug Metab Dispos, volume 36, issue 8, pages 1594-605, Aug 2008, doi 10.1124/dmd.108.020552, PMID 18480186
- Jump up ↑ Y. Jiao, J. Wilkinson, X. Di, W. Wang, H. Hatcher, ND. Kock, R. D'Agostino, MA. Knovich, FM. Torti, Curcumin, a cancer chemopreventive and chemotherapeutic agent, is a biologically active iron chelator., Blood, volume 113, issue 2, pages 462-9, Jan 2009, doi 10.1182/blood-2008-05-155952, PMID 18815282
- Jump up ↑ L. Baum, A. Ng, Curcumin interaction with copper and iron suggests one possible mechanism of action in Alzheimer's disease animal models., J Alzheimers Dis, volume 6, issue 4, pages 367-77; discussion 443-9, Aug 2004, PMID 15345806
- Jump up ↑ R. T. Means, Ironing out complementary medicine, Blood, volume 113, issue 2, 2008, pages 270–271, ISSN 0006-4971, doi 10.1182/blood-2008-10-184630
- Jump up ↑ GE. Goodman, MD. Thornquist, J. Balmes, MR. Cullen, FL. Meyskens, GS. Omenn, B. Valanis, JH. Williams, The Beta-Carotene and Retinol Efficacy Trial: incidence of lung cancer and cardiovascular disease mortality during 6-year follow-up after stopping beta-carotene and retinol supplements., J Natl Cancer Inst, volume 96, issue 23, pages 1743-50, Dec 2004, doi 10.1093/jnci/djh320, PMID 15572756
- Jump up ↑ RA. Sharma, AJ. Gescher, WP. Steward, Curcumin: the story so far., Eur J Cancer, volume 41, issue 13, pages 1955-68, Sep 2005, doi 10.1016/j.ejca.2005.05.009, PMID 16081279
- Jump up ↑ BH. Shah, Z. Nawaz, SA. Pertani, A. Roomi, H. Mahmood, SA. Saeed, AH. Gilani, Inhibitory effect of curcumin, a food spice from turmeric, on platelet-activating factor- and arachidonic acid-mediated platelet aggregation through inhibition of thromboxane formation and Ca2+ signaling., Biochem Pharmacol, volume 58, issue 7, pages 1167-72, Oct 1999, PMID 10484074
- Jump up ↑ David C. Nieman, Lynn Cialdella-Kam, Amy M. Knab, R. Andrew Shanely, Influence of Red Pepper Spice and Turmeric on Inflammation and Oxidative Stress Biomarkers in Overweight Females: A Metabolomics Approach, Plant Foods for Human Nutrition, volume 67, issue 4, 2012, pages 415–421, ISSN 0921-9668, doi 10.1007/s11130-012-0325-x
- ↑ Jump up to: 63.0 63.1 P. Anand, HB. Nair, B. Sung, AB. Kunnumakkara, VR. Yadav, RR. Tekmal, BB. Aggarwal, Design of curcumin-loaded PLGA nanoparticles formulation with enhanced cellular uptake, and increased bioactivity in vitro and superior bioavailability in vivo., Biochem Pharmacol, volume 79, issue 3, pages 330-8, Feb 2010, doi 10.1016/j.bcp.2009.09.003, PMID 19735646
- ↑ Jump up to: 64.0 64.1 Preetha Anand, Ajaikumar B. Kunnumakkara, Robert A. Newman, Bharat B. Aggarwal, Bioavailability of Curcumin: Problems and Promises, Molecular Pharmaceutics, volume 4, issue 6, 2007, pages 807–818, ISSN 1543-8384, doi 10.1021/mp700113r
- Jump up ↑ Reema F. Tayyem, Dennis D. Heath, Wael K. Al-Delaimy, Cheryl L. Rock, Curcumin Content of Turmeric and Curry Powders, Nutrition and Cancer, volume 55, issue 2, 2006, pages 126–131, ISSN 0163-5581, doi 10.1207/s15327914nc5502_2
- Jump up ↑ G. Garcea, DP. Berry, DJ. Jones, R. Singh, AR. Dennison, PB. Farmer, RA. Sharma, WP. Steward, AJ. Gescher, Consumption of the putative chemopreventive agent curcumin by cancer patients: assessment of curcumin levels in the colorectum and their pharmacodynamic consequences., Cancer Epidemiol Biomarkers Prev, volume 14, issue 1, pages 120-5, Jan 2005, PMID 15668484
- ↑ Jump up to: 67.0 67.1 G. Shoba, D. Joy, T. Joseph, M. Majeed, R. Rajendran, PS. Srinivas, Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers., Planta Med, volume 64, issue 4, pages 353-6, May 1998, doi 10.1055/s-2006-957450, PMID 9619120
- Jump up ↑ Mohit Kumar Bhutani, Mahendra Bishnoi, Shrinivas K. Kulkarni, Anti-depressant like effect of curcumin and its combination with piperine in unpredictable chronic stress-induced behavioral, biochemical and neurochemical changes, Pharmacology Biochemistry and Behavior, volume 92, issue 1, 2009, pages 39–43, ISSN 00913057, doi 10.1016/j.pbb.2008.10.007
- Jump up ↑ CA. Arcaro, VO. Gutierres, RP. Assis, TF. Moreira, PI. Costa, AM. Baviera, IL. Brunetti, Piperine, a natural bioenhancer, nullifies the antidiabetic and antioxidant activities of curcumin in streptozotocin-diabetic rats., PLoS One, volume 9, issue 12, pages e113993, 2014, doi 10.1371/journal.pone.0113993, PMID 25469699
- Jump up ↑ D. Suresh, K. Srinivasan, Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats., Indian J Med Res, volume 131, pages 682-91, May 2010, PMID 20516541
- Jump up ↑ CK. Atal, RK. Dubey, J. Singh, Biochemical basis of enhanced drug bioavailability by piperine: evidence that piperine is a potent inhibitor of drug metabolism., J Pharmacol Exp Ther, volume 232, issue 1, pages 258-62, Jan 1985, PMID 3917507
- Jump up ↑ RK. Bhardwaj, H. Glaeser, L. Becquemont, U. Klotz, SK. Gupta, MF. Fromm, Piperine, a major constituent of black pepper, inhibits human P-glycoprotein and CYP3A4., J Pharmacol Exp Ther, volume 302, issue 2, pages 645-50, Aug 2002, doi 10.1124/jpet.102.034728, PMID 12130727
- Jump up ↑ J. Singh, RK. Dubey, CK. Atal, Piperine-mediated inhibition of glucuronidation activity in isolated epithelial cells of the guinea-pig small intestine: evidence that piperine lowers the endogeneous UDP-glucuronic acid content., J Pharmacol Exp Ther, volume 236, issue 2, pages 488-93, Feb 1986, PMID 3080587
- Jump up ↑ Thierry Appelboom, Nathalie Maes, Adelin Albert, A New Curcuma Extract (Flexofytol®) in Osteoarthritis: Results from a Belgian Real-Life Experience, The Open Rheumatology Journal, volume 8, issue 1, 2014, pages 77–81, ISSN 18743129, doi 10.2174/1874312901408010077
- Jump up ↑ A. Bertolini, A. Ottani, M. Sandrini, Selective COX-2 inhibitors and dual acting anti-inflammatory drugs: critical remarks., Curr Med Chem, volume 9, issue 10, pages 1033-43, May 2002, PMID 12733982
- ↑ Jump up to: 76.0 76.1 CJ. Hawkey, COX-1 and COX-2 inhibitors., Best Pract Res Clin Gastroenterol, volume 15, issue 5, pages 801-20, Oct 2001, doi 10.1053/bega.2001.0236, PMID 11566042
- Jump up ↑ N. Futaki, S. Takahashi, M. Yokoyama, I. Arai, S. Higuchi, S. Otomo, NS-398, a new anti-inflammatory agent, selectively inhibits prostaglandin G/H synthase/cyclooxygenase (COX-2) activity in vitro, Prostaglandins, volume 47, issue 1, 1994, pages 55–59, ISSN 00906980, doi 10.1016/0090-6980(94)90074-4
- Jump up ↑ CJ Hawkey, COX-2 inhibitors, The Lancet, volume 353, issue 9149, 1999, pages 307–314, ISSN 01406736, doi 10.1016/S0140-6736(98)12154-2
- Jump up ↑ T. Moini Zanjani, H. Ameli, F. Labibi, K. Sedaghat, M. Sabetkasaei, The Attenuation of Pain Behavior and Serum COX-2 Concentration by Curcumin in a Rat Model of Neuropathic Pain., Korean J Pain, volume 27, issue 3, pages 246-52, Jul 2014, doi 10.3344/kjp.2014.27.3.246, PMID 25031810
- Jump up ↑ K. Moriyuki, F. Sekiguchi, K. Matsubara, H. Nishikawa, A. Kawabata, Curcumin Inhibits the proteinase-activated receptor-2-triggered prostaglandin E2 production by suppressing cyclooxygenase-2 upregulation and Akt-dependent activation of nuclear factor-κB in human lung epithelial cells., J Pharmacol Sci, volume 114, issue 2, pages 225-9, 2010, PMID 20838026
- Jump up ↑ C. Ireson, S. Orr, DJ. Jones, R. Verschoyle, CK. Lim, JL. Luo, L. Howells, S. Plummer, R. Jukes, Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production., Cancer Res, volume 61, issue 3, pages 1058-64, Feb 2001, PMID 11221833
- Jump up ↑ S. Lev-Ari, A. Starr, A. Vexler, V. Karaush, V. Loew, J. Greif, E. Fenig, D. Aderka, R. Ben-Yosef, Inhibition of pancreatic and lung adenocarcinoma cell survival by curcumin is associated with increased apoptosis, down-regulation of COX-2 and EGFR and inhibition of Erk1/2 activity., Anticancer Res, volume 26, issue 6B, pages 4423-30, PMID 17201164
- Jump up ↑ SM. Plummer, KA. Holloway, MM. Manson, RJ. Munks, A. Kaptein, S. Farrow, L. Howells, Inhibition of cyclo-oxygenase 2 expression in colon cells by the chemopreventive agent curcumin involves inhibition of NF-kappaB activation via the NIK/IKK signalling complex., Oncogene, volume 18, issue 44, pages 6013-20, Oct 1999, doi 10.1038/sj.onc.1202980, PMID 10557090
- ↑ Jump up to: 84.0 84.1 84.2 R.S. Ramsewak, D.L. DeWitt, M.G. Nair, Cytotoxicity, antioxidant and anti-inflammatory activities of Curcumins I–III from Curcuma longa, Phytomedicine, volume 7, issue 4, 2000, pages 303–308, ISSN 09447113, doi 10.1016/S0944-7113(00)80048-3
- Jump up ↑ Y. Henrotin, AL. Clutterbuck, D. Allaway, EM. Lodwig, P. Harris, M. Mathy-Hartert, M. Shakibaei, A. Mobasheri, Biological actions of curcumin on articular chondrocytes., Osteoarthritis Cartilage, volume 18, issue 2, pages 141-9, Feb 2010, doi 10.1016/j.joca.2009.10.002, PMID 19836480
- Jump up ↑ Exertional rhabdomyolysis and acute renal failure... [Sports Med. 2007] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/17465608
- ↑ Jump up to: 87.0 87.1 http://journals.lww.com/acsm-csmr/Abstract/2010/03000/Athletes,_NSAID,_Coxibs,_and_the_Gastrointestinal.11.aspx
- Jump up ↑ KIDNEY FAILURE AND ULTRAMARATHONING http://www.lehigh.edu/\~dmd1/kidney.html
- Jump up ↑ Recurrent rhabdomyolysis in a collegiat... [Med Sci Sports Exerc. 2006] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16540825
- Jump up ↑ NSAID Use Increases the Risk of Developing Hyponatremia duri... : Medicine & Science in Sports & Exercise http://journals.lww.com/acsm-msse/Abstract/2006/04000/NSAID_Use_Increases_the_Risk_of_Developing.2.aspx
- Jump up ↑ http://journals.lww.com/cjsportsmed/Abstract/2007/01000/Exercise_Associated_Hyponatremia,_Renal_Function,.8.aspx
- Jump up ↑ http://www.sciencedirect.com/science/article/pii/S0002934307001672
- Jump up ↑ http://journals.lww.com/cjsportsmed/Abstract/2003/01000/The_Incidence,_Risk_Factors,_and_Clinical.8.aspx
- Jump up ↑ CL. Dumke, DC. Nieman, K. Oley, RH. Lind, Ibuprofen does not affect serum electrolyte concentrations after an ultradistance run., Br J Sports Med, volume 41, issue 8, pages 492-6; discussion 496, Aug 2007, doi 10.1136/bjsm.2006.033597, PMID 17331976
- Jump up ↑ FDA Drug Safety Communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes, http://www.fda.gov/Drugs/DrugSafety/ucm451800.htm, Accessed on 25 January 2016
- Jump up ↑ K. Cheung, P. Hume, L. Maxwell, Delayed onset muscle soreness : treatment strategies and performance factors., Sports Med, volume 33, issue 2, pages 145-64, 2003, PMID 12617692
- Jump up ↑ Smith LL. Causes of delayed onset muscle soreness and the impact on athletic performance: a review. J Appl Sport Sci Res 1992; 6 (3): 135-41
- Jump up ↑ A. Baldwin Lanier, Use of nonsteroidal anti-inflammatory drugs following exercise-induced muscle injury., Sports Med, volume 33, issue 3, pages 177-85, 2003, PMID 12656639
- Jump up ↑ G. Howatson, KA. van Someren, The prevention and treatment of exercise-induced muscle damage., Sports Med, volume 38, issue 6, pages 483-503, 2008, PMID 18489195
- Jump up ↑ DK. Mishra, J. Fridén, MC. Schmitz, RL. Lieber, Anti-inflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function., J Bone Joint Surg Am, volume 77, issue 10, pages 1510-9, Oct 1995, PMID 7593059
- ↑ Jump up to: 101.0 101.1 SM. Hasson, JC. Daniels, JG. Divine, BR. Niebuhr, S. Richmond, PG. Stein, JH. Williams, Effect of ibuprofen use on muscle soreness, damage, and performance: a preliminary investigation., Med Sci Sports Exerc, volume 25, issue 1, pages 9-17, Jan 1993, PMID 8423760
- ↑ Jump up to: 102.0 102.1 Tokmakidis SP, Kokkinidis EA, Smilios I, Douda H, The effects of ibuprofen on delayed muscle soreness and muscular performance after eccentric exercise., J Strength Cond Res, 2003, volume 17, issue 1, pages 53-9, PMID 12580656
- ↑ Jump up to: 103.0 103.1 Effect of Ibuprofen Use on Delayed Onset Muscle Soreness of the Elbow Flexors http://journals.humankinetics.com/jsr-back-issues/jsrvolume4issue4november/effectofibuprofenuseondelayedonsetmusclesorenessoftheelbowflexors
- ↑ Jump up to: 104.0 104.1 FX. Pizza, D. Cavender, A. Stockard, H. Baylies, A. Beighle, Anti-inflammatory doses of ibuprofen: effect on neutrophils and exercise-induced muscle injury., Int J Sports Med, volume 20, issue 2, pages 98-102, Feb 1999, doi 10.1055/s-2007-971100, PMID 10190769
- ↑ Jump up to: 105.0 105.1 N Rahnama, F Rahmani-Nia, K Ebrahim, The isolated and combined effects of selected physical activity and ibuprofen on delayed-onset muscle soreness, Journal of Sports Sciences, volume 23, issue 8, 2005, pages 843–850, ISSN 0264-0414, doi 10.1080/02640410400021989
- ↑ Jump up to: 106.0 106.1 Joel R. Krentz, Braden Quest, Jonathan P. Farthing, Dale W. Quest, Philip D. Chilibeck, The effects of ibuprofen on muscle hypertrophy, strength, and soreness during resistance training, Applied Physiology, Nutrition, and Metabolism, volume 33, issue 3, 2008, pages 470–475, ISSN 1715-5312, doi 10.1139/H08-019
- ↑ Jump up to: 107.0 107.1 Lars Arendt-Nielsen, Morten Weidner, Dorte Bartholin, Allan Rosetzsky, A Double-Blind Randomized Placebo Controlled Parallel Group Study Evaluating the Effects of Ibuprofen and Glucosamine Sulfate on Exercise Induced Muscle Soreness, Journal Of Musculoskeletal Pain, volume 15, issue 1, 2007, pages 21–28, ISSN 1058-2452, doi 10.1300/J094v15n01_04
- ↑ Jump up to: 108.0 108.1 AE. Donnelly, RJ. Maughan, PH. Whiting, Effects of ibuprofen on exercise-induced muscle soreness and indices of muscle damage., Br J Sports Med, volume 24, issue 3, pages 191-5, Sep 1990, PMID 2078806
- ↑ Jump up to: 109.0 109.1 109.2 MB. Stone, MA. Merrick, CD. Ingersoll, JE. Edwards, Preliminary comparison of bromelain and Ibuprofen for delayed onset muscle soreness management., Clin J Sport Med, volume 12, issue 6, pages 373-8, Nov 2002, PMID 12466693
- Jump up ↑ Robert D. Hyldahl, Justin Keadle, Pierre A. Rouzier, Dennis Pearl, Priscilla M. Clarkson, Effects of Ibuprofen Topical Gel on Muscle Soreness, Medicine & Science in Sports & Exercise, volume 42, issue 3, 2010, pages 614–621, ISSN 0195-9131, doi 10.1249/MSS.0b013e3181b95db2
- ↑ Jump up to: 111.0 111.1 111.2 P. Barlas, JA. Craig, J. Robinson, DM. Walsh, GD. Baxter, JM. Allen, Managing delayed-onset muscle soreness: lack of effect of selected oral systemic analgesics., Arch Phys Med Rehabil, volume 81, issue 7, pages 966-72, Jul 2000, doi 10.1053/apmr.2000.6277, PMID 10896014
- ↑ Jump up to: 112.0 112.1 Lucille Smith, Robert George, Thomas Chenier, Michael McCammon, Joseph Houmard, Richard Israel, R. A. Hoppmann, Susan Smith, Do over-the-counter analgesics reduce delayed onset muscle soreness and serum creatine kinase values?, Research in Sports Medicine, volume 6, issue 2, 1995, pages 81–88, ISSN 1543-8627, doi 10.1080/15438629509512039
- ↑ Jump up to: 113.0 113.1 Riasati et al.: Aspirin and delayed onset muscle soreness ASPIRIN MAY BE AN EFFECTIVE TREATMENT FOR EXERCISE- INDUCED MUSCLE SORENESS | ResearchGate http://www.researchgate.net/publication/228091056_Riasati_et_al._Aspirin_and_delayed_onset_muscle_soreness_ASPIRIN_MAY_BE_AN_EFFECTIVE_TREATMENT_FOR_EXERCISE-_INDUCED_MUSCLE_SORENESS
- ↑ Jump up to: 114.0 114.1 KT. Francis, T. Hoobler, Effects of aspirin on delayed muscle soreness., J Sports Med Phys Fitness, volume 27, issue 3, pages 333-7, Sep 1987, PMID 3431117
- ↑ Jump up to: 115.0 115.1 GA. Dudley, J. Czerkawski, A. Meinrod, G. Gillis, A. Baldwin, M. Scarpone, Efficacy of naproxen sodium for exercise-induced dysfunction muscle injury and soreness., Clin J Sport Med, volume 7, issue 1, pages 3-10, Jan 1997, PMID 9117523
- ↑ Jump up to: 116.0 116.1 AC. Baldwin, SW. Stevenson, GA. Dudley, Nonsteroidal anti-inflammatory therapy after eccentric exercise in healthy older individuals., J Gerontol A Biol Sci Med Sci, volume 56, issue 8, pages M510-3, Aug 2001, PMID 11487604
- ↑ Jump up to: 117.0 117.1 JM. Lecomte, VJ. Lacroix, DL. Montgomery, A randomized controlled trial of the effect of naproxen on delayed onset muscle soreness and muscle strength., Clin J Sport Med, volume 8, issue 2, pages 82-7, Apr 1998, PMID 9641434
- Jump up ↑ The Effect of Taking Naproxen Drug on the Level of Perceived Pain and Changes of CPK Serum after Eccentric Exercise - Harakat Volume: 37, Issue:, Accessed on 3 January 2013
- ↑ Jump up to: 119.0 119.1 J. Bourgeois, D. MacDougall, J. MacDonald, M. Tarnopolsky, Naproxen does not alter indices of muscle damage in resistance-exercise trained men., Med Sci Sports Exerc, volume 31, issue 1, pages 4-9, Jan 1999, PMID 9927002
- Jump up ↑ A E Donnelly, K McCormick, R J Maughan, P H Whiting, P M Clarkson, Effects of a non-steroidal anti-inflammatory drug on delayed onset muscle soreness and indices of damage., British Journal of Sports Medicine, volume 22, issue 1, 1988, pages 35–38, ISSN 0306-3674, doi 10.1136/bjsm.22.1.35
- Jump up ↑ L.C. Loram, D. Mitchell, A. Fuller, Rofecoxib and tramadol do not attenuate delayed-onset muscle soreness or ischaemic pain in human volunteers, Canadian Journal of Physiology and Pharmacology, volume 83, issue 12, 2005, pages 1137–1145, ISSN 0008-4212, doi 10.1139/y05-113
- ↑ Jump up to: 122.0 122.1 SP. Sayers, CA. Knight, PM. Clarkson, EH. Van Wegen, G. Kamen, Effect of ketoprofen on muscle function and sEMG activity after eccentric exercise., Med Sci Sports Exerc, volume 33, issue 5, pages 702-10, May 2001, PMID 11323536
- Jump up ↑ K. van Wijck, K. Lenaerts, LJ. van Loon, WH. Peters, WA. Buurman, CH. Dejong, Exercise-induced splanchnic hypoperfusion results in gut dysfunction in healthy men., PLoS One, volume 6, issue 7, pages e22366, 2011, doi 10.1371/journal.pone.0022366, PMID 21811592
- Jump up ↑ K. VAN Wijck, K. Lenaerts, AA. VAN Bijnen, B. Boonen, LJ. VAN Loon, CH. Dejong, WA. Buurman, Aggravation of exercise-induced intestinal injury by Ibuprofen in athletes., Med Sci Sports Exerc, volume 44, issue 12, pages 2257-62, Dec 2012, doi 10.1249/MSS.0b013e318265dd3d, PMID 22776871
- Jump up ↑ IC. Vermeulen Windsant, FA. Hellenthal, JP. Derikx, MH. Prins, WA. Buurman, MJ. Jacobs, GW. Schurink, Circulating intestinal fatty acid-binding protein as an early marker of intestinal necrosis after aortic surgery: a prospective observational cohort study., Ann Surg, volume 255, issue 4, pages 796-803, Apr 2012, doi 10.1097/SLA.0b013e31824b1e16, PMID 22367448
- Jump up ↑ Wayne K. Stadelmann, Alexander G. Digenis, Gordon R. Tobin, Impediments to wound healing, The American Journal of Surgery, volume 176, issue 2, 1998, pages 39S–47S, ISSN 00029610, doi 10.1016/S0002-9610(98)00184-6
- Jump up ↑ S. Guo, L. A. DiPietro, Factors Affecting Wound Healing, Journal of Dental Research, volume 89, issue 3, 2010, pages 219–229, ISSN 0022-0345, doi 10.1177/0022034509359125
- Jump up ↑ Ibuprofen use during extreme exercise: ... [Med Sci Sports Exerc. 2007] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/17596774
- Jump up ↑ Ibuprofen use, endotoxemia, inflammation, ... [Brain Behav Immun. 2006] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16554145
- Jump up ↑ Ibuprofen Official FDA information, side effects and uses. http://www.drugs.com/pro/ibuprofen.html
- Jump up ↑ Ibuprofen/Famotidine Reduces Gastric Ulcer Incidence http://www.medscape.com/viewarticle/732432
- Jump up ↑ Acetaminophen-induced acute liver failure: Results of a United States multicenter, prospective study - Larson - 2005 - Hepatology - Wiley Online Library http://onlinelibrary.wiley.com/doi/10.1002/hep.20948/pdf
- ↑ Jump up to: 133.0 133.1 133.2 133.3 Staggered overdose pattern and delay to hospital presentation are associated with adverse outcomes following paracetamol-induced hepatotoxicity http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2125.2011.04067.x/full
- Jump up ↑ FDA May Restrict Acetaminophen http://www.webmd.com/pain-management/news/20090701/fda-may-restrict-acetaminophen
- Jump up ↑ ACETAMINOPHEN (PARACETAMOL) http://www.chemicalland21.com/lifescience/phar/ACETAMINOPHEN.htm
- Jump up ↑ GG. Graham, KF. Scott, Mechanism of action of paracetamol., Am J Ther, volume 12, issue 1, pages 46-55, PMID 15662292
- Jump up ↑ Regina Botting, Samir S. Ayoub, COX-3 and the mechanism of action of paracetamol/acetaminophen, Prostaglandins, Leukotrienes and Essential Fatty Acids, volume 72, issue 2, 2005, pages 85–87, ISSN 09523278, doi 10.1016/j.plefa.2004.10.005
- Jump up ↑ K. Toussaint, X. C. Yang, M. A. Zielinski, K. L. Reigle, S. D. Sacavage, S. Nagar, R. B. Raffa, What do we (not) know about how paracetamol (acetaminophen) works?, Journal of Clinical Pharmacy and Therapeutics, volume 35, issue 6, 2010, pages 617–638, ISSN 02694727, doi 10.1111/j.1365-2710.2009.01143.x
- Jump up ↑ Brian J. Anderson, Paracetamol (Acetaminophen): mechanisms of action, Pediatric Anesthesia, volume 18, issue 10, 2008, pages 915–921, ISSN 11555645, doi 10.1111/j.1460-9592.2008.02764.x
- Category:Training
- Category:Injury
- Category:Science

