Iliotibial band syndrome (ITBS)
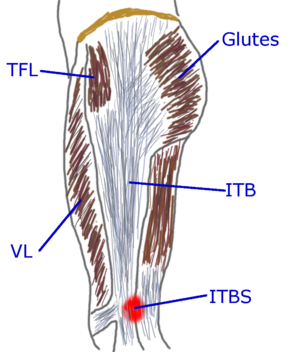
Iliotibial band syndrome (ITBS) generally causes pain in the outside of the knee, with the pain often arising after a couple of miles of running. The Iliotibial band (ITB) runs from the crest of the hip bone (Iliac) to the top of the shin bone (tibia) near the knee, hence the name. ITBS is a common issue for runners, with research suggesting it impacts about a 6thof all runners[1]. Sometimes runners ITBS is confused with pain under the kneecap, but ITBS is normally specific to a small area on the outside of the knee, and is most noticeable when the knee is flexed to 30 degrees. There are a number of possible approaches to treating ITBS, but even with the numerous research studies into ITBS, the quality of information is remarkably limited[2].
- The TFL. I have found the most effective treatment for ITBS is to focus on the Tensor Fasciae Latae (TFL). I use the Thumper to Massage the TFL, which can be quite painful, but works well, as massaging with my fingers. This massage should be combined with strengthening the TFL. One of the best exercises for this is the 'Frankenstein march'. To do this you will need a short resistance band like this Error: Could not parse data from Amazon!. Put the band around your ankles and walk with your feet about shoulder with apart. You need enough tension on the strap so that when you walk, you have to put an effort into keeping your feet apart. Walk a short distance, keeping your feet pointing straight ahead. Go far enough that you can feel the effort in your hips, but don't overdo it.
- The Glutes. The TFL/ITB generally works together with your glutes, so if the glutes are weak, the TFL/ITB has to work harder. The hip abductors are your glutes (Gluteus Maximus, Gluteus Medius, & Gluteus Minimus), plus the TFL. The word "abduct" means to "lead away" and the hip abductors pull your legs outwards, away from your midline. Like the TFL, the Glutes need Massage and strengthened. The Frankenstein March also works to strengthen the Glutes.
- Mobilize the ITB. Massage of the ITB from the hip to the knee can help mobilize the ITB. Using the Foam Roller to massage the outside of the thigh can be quite painful, so using your other leg to reduce the pressure is often needed to keep things bearable. You can also use your hand to massage the ITB and surrounding muscles (vastus lateralis and biceps femoris.)
- Ice. Using Ice on the site of the pain can help reduce the swelling and pain, but it does not seem to help address the root cause. You can also ice the TFL, which may be more effective.
- Avoid NDADs. NSAIDs like ibuprofen will help mask the pain and can reduce the inflammation of ITBS, but they can also retard the healing process.
- Replace Your Shoes. It is possible for badly worn Shoes to change your biomechanics enough to trigger ITBS. It's worth checking your Shoes for excessive wear; not the tread on the outsole, but the midsole foam. Feel the thickness of the sole and see if it is significantly thinner in some sections, such as where the ball of the foot presses.
- Biomechanics. Poor biomechanics can cause ITBS, so having someone evaluate your Running Form may help. Another approach is to have someone video tape your running and check it for good form. You should check your Cadence, as the correct Cadence can resolve many biomechanical issues like Overstriding.
- Avoid Fuel Belts. Though the pain of ITBS is felt near the knee, the origin of the ITBS is at the hip. Therefore anything that presses on the ITB high on the leg, or worse the TFL, can cause or aggravate ITBS. If you have been wearing a fuel belt, or any other type of belt around the hips, I'd recommend not wearing it until the ITBS has completely recovered. If you feel the fuel belt is worth it, try reintroducing it and see if the ITBS reoccurs.
- Foot angle. Personally, I've found that if my feet are turned even slightly outwards (AKA lateral rotation or duck feet) it can trigger ITBS quite rapidly. I suspect this is because this outward rotation causes the knee to tend to bend inwards and the muscles have to pull on the ITB to maintain stability.
References
- Jump up ↑ B. Noehren, I. Davis, J. Hamill, ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome., Clin Biomech (Bristol, Avon), volume 22, issue 9, pages 951-6, Nov 2007, doi 10.1016/j.clinbiomech.2007.07.001, PMID 17728030
- Jump up ↑ Jodi Aderem, Quinette A. Louw, Biomechanical risk factors associated with iliotibial band syndrome in runners: a systematic review, BMC Musculoskeletal Disorders, volume 16, issue 1, 2015, ISSN 1471-2474, doi 10.1186/s12891-015-0808-7
- Category:Injury