Knee Pain
A pain behind the kneecap is one of the most problems for runners[1], so much so that it is sometimes referred to as 'runners knee'[2]. There is no well-established cure for this problem[3], but there are a number of things you can try and some treatments to avoid. (Note that there are other types of pain in and around the knee, but this article only looks at pain behind the kneecap, more properly called Patellofemoral pain syndrome or PFPS,)
Contents
1 Causes
There are a number of possible root causes of knee pain.
1.1 Excessive stress
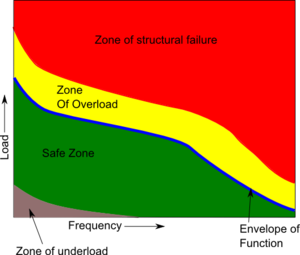
The kneecap is an amazing structure, but like all body parts, it has limits in the load it can take. This overload may be due to a number of factors.
- Low Cadence. Having a low Cadence results in more vertical movement, and thus higher landing forces.
- Highly cushioned shoes. Counterintuitively, the more cushioned your shoes are, the greater the loading force on your knees[4][5].
- Obesity. Obviously being overweight puts more stress on the knees and is linked to knee pain[6].
- Bad running form. Problems with running form can increase the landing forces and cause injury.
- Overstriding. Overstriding is landing with the foot ahead of the hip, can increase the landing forces and cause injury[7]. (See Are You Overstriding? and An Analysis of Running Technique for details on overstriding.)
- Heel strike. Landing with the weight on the heel of the foot creates a far greater peak force than landing so the weight is taken by the midfoot or forefoot [8].
1.2 Inactivity
The human body needs activity to remain healthy, and the knee is a prime example of this. Animal studies have shown than complete immobilization of the knee can result in a 50% reduction in the cartilage thickness within weeks[9]. Thankfully this damage appears to be reversible.
1.3 Weak Quads
It is common for people with knee pain to have weak quads[10]. However, I have found no research to suggest that weak quads are a cause of knee pain, a rather than a result of knee pain. I believe that it is more reasonable to conclude that knee pain results in less exercise as the patient avoids activities that cause pain, and thus the quads become weaker through inactivity.
1.4 Maltracking/malalignment
The kneecap moves in a groove in the thigh bone (femur), and it is widely believed[11] that if the kneecap does not track in this grove it will rub on the sides and cause knee pain. While this belief is not well supported by the evidence[12], the following underlying problems may still cause knee pain through other mechanisms.- Weak VMO. The alignment of the kneecap is not related to the overall strength of the quads, but rather an imbalance of the muscles that make up the quads. The quads consist of four muscles, and a relative weakness in a subdivision of one muscle, the Vastus Medialis Obliquus or VMO, has been linked to kneecap alignment[13] and knee pain[14].
- VMO Delay. There is some evidence that people suffering from knee pain (PFPS) have a delay in the activation of the VMO compared with the main quad muscles[15][16], which reduced the lateral force by 25%[17]. Detecting this timing difference is normally requires sophisticated clinical equipment, but there is some suggestion that the delay can be felt directly by placing fingers on the belly of the VMO and the VL[10].
- Weak Hips. A weakness in the hip muscles has been linked to knee pain[18]. Weak hip muscles result in the leg rotating so the foot points towards the midline of the body (internal rotation), so when the leg bends extra stress is placed on the knee.
- Q Angle. The thigh bone and lower leg are not in a straight line, but form an angle at the knee called the 'Q Angle'. A large Q Angle is often thought to cause or contribute to knee pain, but a high Q angle was only seen in 6% of knee pain (PFPS) cases[1] and a high Q Angle is not associated with biomechanical knee stress[19].
- Over Pronation. Pronation is the natural movement of the foot where the arch flattens to absorb landing forces. If the foot pronates too much, the foot will lean towards the midline of the body and the lower leg and knee will follow this motion, moving towards the midline. Like weak hips, the movement of the knee towards the midline creates extra stress on the knee.
1.5 Arthritis
Arthritis is an inflammation of the joints and can affect the knee. There are various types of arthritis, and diagnosis requires X-Ray, testing the fluid around the joint or inserting a viewing scope into the joint. Arthritis is outside of the scope of this article.
1.6 Baker's cyst
A baker's cyst causes pain behind the knee joint rather than under the knee cap.
1.7 ITBS
Another common source of knee pain is Iliotibial band syndrome which generally causes pain to the outside of the knee.
1.8 Fracture
A fracture of the kneecap will obviously cause knee pain, but is normally the result of trauma. If you suspect you have a fractured kneecap, seek medical help.
1.9 NSAIDs
Cartilage destruction is a major cause of concern with NSAIDs[20], but I found no long term studies that link NSAID use with knee problems, so it's not clear if this is a widespread cause of knee pain.
1.10 Chondromalacia
The term Chondromalacia means soft cartilage and was once thought to be a common cause of knee pain. However, studies have shown that people with advanced Chondromalacia can be pain free[3].
1.11 Leg length discrepancy
A difference in leg length can be a factor in knee pain[10].
2 Treatments
This list is roughly in order of the viability and priority of the treatments.
- Reduce Knee Stress. Stress on the knee should be reduced to prevent further damage[10]. Personally, I do not believe in complete rest, but prefer reduced exercise, trying to avoid or minimize pain as I believe the exercise promotes healing.
- Ice. The use of ice will not remove the underlying cause of knee pain, but it can help with recovery and healing. See Cryotherapy for more details.
- Cadence. If you're cadence is too low it can cause various problems, and should be optimized to around 180 steps per minute (90 steps/min for each leg). See Cadence for more details.
- Massage the VMO. While the evidence for weak quads and VMO is marginal, massaging the VMO is easy and reasonably risk free. While the [[Foam Roller] is good for massaging most of the quads, it tends not to get to the VMO, and if the Foam Roller is your only quad massage technique then it's possible that your VMO is suffering from neglect. I would recommend using The Stick as well as using your elbow on the VMO. I've also found that using an electronic muscle stimulator on the VMO can help. See main article on Massage for more details.
- Massage the glutes. Weak glute muscles have been linked to knee pain[18][21], so massaging them may help them recover their strength and functionality.
- Electrical Muscle Stimulation. Strengthening the quad muscles using normal resistance training tends to put extra stress on the kneecap aggravating the injury. Resistance training the quad muscles tends to equally train all parts, rather than focusing on the VMO. The only known way to selectively strengthen the VMO is by the use of Electrical Muscle Stimulation[10]. See Electrical Muscle Stimulation for more details.
- Footwear. There are two types of footwear changes that may help with knee pain that are contradictory; minimalist footwear and orthotics. Personally, I am concerned that Orthotics may help with knee pain but cause other problems, and the use of orthotics goes against the evidence for minimalist footwear. However, there is more scientific evidence to support orthotics for resolving knee pain, even though orthotics may increase knee stress. My personal belief is that it is better to cautiously move towards Minimalist Running Footwear rather than use orthotics, but I want to be clear that there is not clear scientific support for my belief.
- Minimalist shoes. There is good evidence that running shoes increase the stress on the knee[22], and that a more minimalist approach to footwear may be appropriate. There is plenty of anecdotal evidence[23] that minimalist footwear helps with knee pain, but only limited science[24] to back it up. Also, changing too quickly to minimalist footwear may result in Too Much Too Soon injuries. See 'Are your running shoes injuring you?' for more details.
- Orthotics. Studies have shown that orthotics reduce knee pain, with a greater benefit shown in those that have greater pronation[25][26][27]. However, there are concerns that orthotics may also increase the stress on the knee[28].
- Running form. Good running form has many benefits, but changing form tends to be difficult and can easily result in new injuries if done too quickly. I would recommend looking at Chi Running or the Pose Method, though personally I don't agree with their approach of pure forefoot running (your heal not touching the ground) and prefer a midfoot strike.
- Check for ITBS. ITBS produces pain to the outside of the knee, rather than under the kneecap. It's possible to have both kneecap pain and ITBS, so read Iliotibial band syndrome.
- Taping. The use of tape has been shown to be effective at reducing knee pain[29][30][31], by over 90% in one study[32]. One study used tape to pull the knee cap towards the midline of the body[33], others relied on evaluation to define the correct direction[30]. The most common method mentioned is 'McConnell taping'[31][30], and instructions can be found by Googling 'McConnell taping'.
- VMO Re-timing. If the firing of your VMO is delayed, it may be possible to correct this. Ideally, the correction uses a combination of training and down in EMG biofeedback device. These devices can be quite expensive, but it may be possible to detect the difference in timing between the VMO and the VL using your fingertips[10]. The goal should be retraining control rather than strengthening, with 200 repetitions per day (20x 10 reps) being required[10]. (I did find instructions for a DIY EMG.)In addition, it may be possible to mitigate the VMO timing problem with taping[29][31] (see below).
- Joint Supplements. The joint supplements glucosamine and chondroitin provide marginal benefit, but are considered safe, so they may be worth considering if you can justify the expense. Other supplements such as Omega 3 oils and Vitamin C/E may be worth considering. For more details, see Joint Supplements.
- Knee brace/sleeve/strap. A knee sleeve is a simple elastic wrap that goes around the knee, sometimes with a hole to avoid pressure on the kneecap. A knee brace usually provides hard plastic support in addition to the sleeve. The evidence supporting knee braces is limited[34][35], with many of the studies having poor quality[35]. One reasonable study showed improvement with a brace[36], but better quality studies showed no benefit[37][38][39]. There are even fewer studies for knee sleeves[40]. The only study on knee straps showed no benefit[37]. I found no indications of the long term effects or safety of knee braces, sleeves or straps. Based on the available evidence, the use of these approaches does not seem justified. I found no studies that looked at Compression Tights but they may act in a similar way to a knee sleeve and they have other benefits.
3 Anti-treatments
The following 'treatments' are not recommended.
- Quad resistance training. A common recommendation is to strengthen the quad muscles to improve the tracking of the kneecap, especially the VMO. However, resistance training of the quads puts extra strain on the kneecap and can cause a worsening of the symptoms[3].
- Surgery to correct mistracking. A study of knee pain indicated that this type of surgery has the second highest failure rate[3].
- NSAIDs. Using NSAIDs does not generally improve healing, can mask symptoms and is a cause of cartilage damage[20]. An animal study showed that Asprin resulted in greater cartilage degeneration[41]. More at NSAIDs and Running.
4 References
- ↑ 1.0 1.1 A retrospective case-control analysis of 2002 running injuries -- Taunton et al. 36 (2): 95 -- British Journal of Sports Medicine http://bjsm.bmj.com/content/36/2/95
- ↑ Runner's Knee (Patellofemoral Pain) - OrthoInfo - AAOS http://orthoinfo.aaos.org/topic.cfm?topic=a00382
- ↑ 3.0 3.1 3.2 3.3 Patellofemoral Pain Current Concepts: An Overview : Sports Medicine and Arthroscopy Review http://journals.lww.com/sportsmedarthro/Abstract/2001/10000/Patellofemoral_Pain_Current_Concepts__An_Overview.2.aspx
- ↑ Minimalist Footwear http://antonkrupicka.blogspot.com/2007/10/minimalist-footwear.html
- ↑ Factors related to the incidence of running injuries. A review. http://www.ncbi.nlm.nih.gov/pubmed/1615258
- ↑ THE ASSOCIATION OF KNEE INJURY AND OBESITY WITH UNILATERAL AND BILATERAL OSTEOARTHRITIS OF THE KNEE http://aje.oxfordjournals.org/content/130/2/278.short
- ↑ Mechanisms of Selected Knee Injuries http://physicaltherapyjournal.com/content/60/12/1590.short
- ↑ Landing Pattern Modification to Improve Patellofemoral Pain in Runners: A Case Series - JOSPT – Journal of Orthopaedic & Sports Physical Therapy http://www.jospt.org/issues/articleID.2653/article_detail.asp
- ↑ Response of joint structures to inactivity and to reloading after immobilization - Brandt - 2003 - Arthritis Care & Research - Wiley Online Library http://onlinelibrary.wiley.com/doi/10.1002/art.11009/full
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 Clinical classification of patellofemoral pain syndrome- guidelines for non-operative treatment, Erik Witvrouw, S. Werner, C. Mikkelsen, D. Van Tiggelen, L. Vanden Berghe, G. Cerulli
- ↑ Knee Injuries From Running at Runner's World.com http://www.runnersworld.com/article/0,7120,s6-241-285--7773-0,00.html
- ↑ The role of patellar alignment and tracking in vivo: The potential mechanism of patellofemoral pain syndrome http://www.sciencedirect.com/science/article/pii/S1466853X11000162
- ↑ Role of the vastus medialis obliquus in repo... [Am J Sports Med. 2008] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/18337358
- ↑ Vastus Medialis Obliquus Atrophy: Does It Exist in Patellofemoral Pain Syndrome? http://ajs.sagepub.com/content/early/2011/04/12/0363546511401183
- ↑ http://rsi.aip.org/resource/1/rsinak/v82/i10/p105101_s1?isAuthorized=no
- ↑ The relative timing of VMO and VL in the aetiology of anterior knee pain: a systematic review and meta-analysis http://www.biomedcentral.com/1471-2474/9/64
- ↑ The quadriceps function in patellofe... [Arch Orthop Trauma Surg. 1987] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/3606363
- ↑ 18.0 18.1 Hip strength and hip and knee kine... [J Orthop Sports Phys Ther. 2008] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/18349475
- ↑ Greater Q angle may not be a ri... [Clin Biomech (Bristol, Avon). 2011] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/21177007
- ↑ 20.0 20.1 ScienceDirect.com - The American Journal of Medicine - Profile and mechanisms of gastrointestinal and other side effects of nonsteroidal anti-inflammatory drugs (NSAIDs) http://www.sciencedirect.com/science/article/pii/S0002934399003654
- ↑ Gluteal muscle activation durin... [Clin Biomech (Bristol, Avon). 2011] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/21388728
- ↑ The Effect of Running Shoes on Lower Extremity Joint Torques http://www.pmrjournal.org/article/S1934-1482(09)01367-7/fulltext
- ↑ Minimalism Case Studies | Running Times Magazine http://runningtimes.com/Article.aspx?ArticleID=22192
- ↑ Joint loading decreased by inexpensive and minimalist footwear in elderly women with knee osteoarthritis during stair descent - Sacco - 2012 - Arthritis Care & Research - Wiley Online Library http://onlinelibrary.wiley.com/doi/10.1002/acr.20690/abstract
- ↑ Application of wedged foot orthosis effectively reduces pain in runners with pronated foot: a randomized clinical study http://cre.sagepub.com/content/early/2011/07/16/0269215511411938.abstract
- ↑ The immediate effects of foot orthoses on fu... [Br J Sports Med. 2011] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/20647297
- ↑ A randomised control trial of short term eff... [Br J Sports Med. 2012] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/21930514
- ↑ Effect of footwear on the external knee adduction momen... [Knee. 2012] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/21733696
- ↑ 29.0 29.1 The management of chondromalacia patellae: a long term solution http://svc019.wic048p.server-web.com/ajp/vol_32/4/AustJPhysiotherv32i4McConnell.pdf
- ↑ 30.0 30.1 30.2 Effects of patella taping on patella po... [Med Sci Sports Exerc. 1993] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/8231783
- ↑ 31.0 31.1 31.2 The effect of patellar taping on the onset of vast... [Phys Ther. 1998] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/9442193
- ↑ Effect of taping the pat... [Knee Surg Sports Traumatol Arthrosc. 1993] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/8536023
- ↑ Taping the patella medially: a new treatment for osteoarthritis of the knee joint? | BMJ http://www.bmj.com/content/308/6931/753.full
- ↑ Braces and orthoses for treating ... [Cochrane Database Syst Rev. 2005] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/15674927
- ↑ 35.0 35.1 Patellar taping and bracing for the treatment of chronic knee pain: A systematic review and meta-analysis - Warden - 2007 - Arthritis Care & Research - Wiley Online Library http://onlinelibrary.wiley.com/doi/10.1002/art.23242/full
- ↑ The effect of bracing on patella alignm... [Med Sci Sports Exerc. 2004] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/15235330
- ↑ 37.0 37.1 The efficacy of orthotics for anterior knee p... [Am J Knee Surg. 1997] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/9051172
- ↑ Effectiveness of patellar bracing for treat... [Clin J Sport Med. 2005] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16003037
- ↑ A randomized trial of patellofemora... [Osteoarthritis Cartilage. 2011] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/21232620
- ↑ Clinical practice guidelines for rest ortho... [Joint Bone Spine. 2009] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/19467901
- ↑ In vivo effect of aspirin on canine osteoarthritic cartilage - Palmoski - 2005 - Arthritis & Rheumatism - Wiley Online Library http://onlinelibrary.wiley.com/doi/10.1002/art.1780260808/abstract