Should you run with a cold or other illness?
Should you run with a cold or other illness? How does running affect your immune system? Does it make it better or worse? The answers to these questions are as complex as the human body itself, but there are some simplified guidelines that can help in most situations. Only use these guidelines if you feel well enough to train and want to train; if in doubt, avoid exercise and rest up.
| Training Style | Mild Cold | More serious infection |
|---|---|---|
| General fitness and health (light training, but no speed work or endurance training and never exhaustive.) |
Train as normal if symptoms are 'above the neck', otherwise reduce the amount of running. | Reduce the amount of running. |
| Structured training (Specific speed and endurance training, but not pushing your physical limits.) |
Avoid exhaustive training during cold. The risk of Overtraining Syndrome is slightly elevated. | Exhaustive training should be avoided for a month after infection. Curtail the intensity and/or length of harder workouts. The risk of Overtraining Syndrome is moderately elevated. |
| Competitive training (Pushing the boundaries of your physical capabilities.) |
During the cold avoid exhaustive training and reduce the intensity and volume of training. The risk of Overtraining Syndrome is moderately elevated. | Exhaustive training should be avoided for a month after infection. Significantly reduce the intensity and volume of training while symptomatic, ramping back up afterwards carefully. The risk of Overtraining Syndrome is significantly elevated. |
Important note: chest pains (especially stabbing pains) or unusual shortness of breath may be symptoms of Myocarditis, a potentially fatal condition.
Contents
[hide]1 Running with a cold or other illness
The common cold (often called Upper Respiratory Tract Infections or URTI in research) is one of the most common problem effecting athletes[1] and some claim it causes more problems than all other illness combined[2]. However, there are other more serious infections that should also be considered.
- Exhaustive exercise compromises the immune system and can make an existing infection worse[3].
- Light exercise while suffering from a mild infection is generally believed to be safe[3]. There is a widespread medical opinion that it's okay to run if the symptoms are all 'above the neck'[4], but there appears to be little or no research to back up this belief.
- Even a mild infection adds to the overall stress levels and increases the risk of Overtraining Syndrome. In addition, an infection may be a symptom of Overtraining Syndrome[3].
- Infection from Rhinovirus (the usual cause of the common cold) does not affect exercise performance[5]. However, it can be tricky to know if an infection is due to the Rhinovirus or some other agent.
- Some infections, such as those involving inflammation of the heart (myocarditis), can be potentially fatal when combined with exercise[6].
- Many infections will reduce performance, sometimes dramatically[7].
- Exhaustive training should be avoided for a month after infection, except for mild common colds [6].
2 Avoiding Infections
- Be aware of the factors causing Overtraining Syndrome, as this can result in a compromised immune system. Factors include life stresses, diet, Training Monotony, and adequate sleep.
- Avoid touching your eyes or nose without first washing your hands, as this is a common route for infectious diseases.
- Where possible keep away from sick people and large crowds when your immune system is likely to be weakened.
- Exhaustive exercise compromises the immune system and can make the athlete more susceptible to infection. Taking carbohydrate before during and after exhaustive exercise can reduce the suppression of the immune system[3].
- Be particularly careful after exhaustive exercise, including racing.
- Monitor Mood State, as this is can be an indication of reduced immune system functioning amongst other things.
3 Running and the immune system
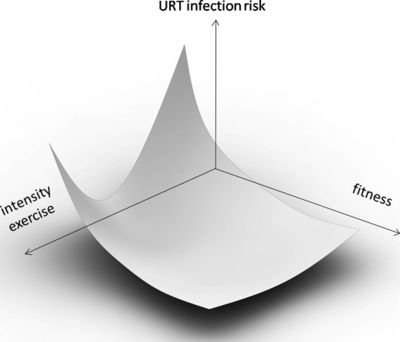
There is a general belief in a 'J' shaped relationship between exercise level and risk of infection[7], but it seems that the shape depends on the level of fitness[8]. Lower fitness individuals' immune system benefits from some exercise, but as the intensity rises, the immune system benefits decline.
4 Racing and the immune system
Races up to and including the half marathon do not have an increased risk of infection[9], but the risk is significantly higher after marathon[10] and ultramarathon[11] races. However, there is some evidence that those experiencing an infection after the marathon distance may be due to a reoccurrence of symptoms from an earlier infection[12].
5 Nutrition and the immune system
There are various supliments that may help improve immune system functioning in runners.
- The amino acid glutamine is required by some parts of the immune system[13](lymphocytes) and exercise depletes blood glutamine levels [14]. There is some evidence that glutamine supplementation is effective at reducing the immune system compromise[15].
- Vitamin C has been shown to reduce the incidence of UTRI by half[16][17][18]. The doses used in the studies were 600mg or 1000mg daily. However, other studies[19] have failed to show a benefit.
- Adding Vitamin E to Vitamin C supplementation does not appear to further enhance the benefit of Vitamin C[17]. However, there may be other benefits from the combination of Vitamin C and E together, such as reduction in the risk of Alzheimer's disease[20].
- There is some evidence[21] that probiotics (e.g. live yoghurt) prevents or reduces the intensity of UTRI symptoms. However, this benefit was not seen in other studies [22], nor did probiotics show a reduction in allergy or asthma symptoms [23].
- Tea, especially green tea, contains Theanine which may help reduce the immune system depression of high intensity training[24][25].
- Taking carbohydrate before during and after exhaustive exercise can reduce the suppression of the immune system[3].
6 Other treatments
- For colds (upper respiratory tract infections), sinus flushing may help reduce the symptoms[26].
7 References
- Jump up ↑ Casey JM, Dick EC. Acute respiratory infections. In: Casey JM, Foster C, Hixson EG, eds. Winter Sports Medicine. Philadelphia, PA: FA Davis Co; 1990:112-128.
- Jump up ↑ Sport, Exercise, and the Common Cold, Thomas G. Weidner, PhD, ATC; Thomas L. Sevier, MD http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1318446/pdf/jathtrain00018-0060.pdf
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Overtraining In Sport, Kreider, Fry, O'Toole, Human Kinetics
- Jump up ↑ Exercise and illness: Work out with a cold? - MayoClinic.com http://www.mayoclinic.com/health/exercise/AN01097
- Jump up ↑ http://journals.lww.com/acsm-msse/Abstract/1997/05000/Effect_of_a_rhinovirus_caused_upper_respiratory.3.aspx
- ↑ Jump up to: 6.0 6.1 Viral illnesses and sports performance. [Sports Med. 1986 Jul-Aug] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/3526508
- ↑ Jump up to: 7.0 7.1 Immunology and Cell Biology - Infections and exercise in high-performance athletes http://www.nature.com/icb/journal/v78/n5/full/icb200071a.html
- ↑ Jump up to: 8.0 8.1 Does exercise increase the risk of upper respiratory tract infections? http://bmb.oxfordjournals.org/content/90/1/111.full
- Jump up ↑ Infectious episodes in runners bef... [J Sports Med Phys Fitness. 1989] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/2635263?dopt=Abstract
- Jump up ↑ Infectious episodes in runners bef... [J Sports Med Phys Fitness. 1990] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/2266764
- Jump up ↑ Ultramarathon running and upper respiratory trac... [S Afr Med J. 1983] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/6623247?dopt=Abstract
- Jump up ↑ Infectious episodes before and after ... [Scand J Med Sci Sports. 2006] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/16895535?dopt=Abstract
- Jump up ↑ Lymphocyte proliferation modulated by glutamine: involved in the endogenous redox reaction http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1905365/
- Jump up ↑ Depression of plasma glutamine concentration afte... [Med J Aust. 1995] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/7845291
- Jump up ↑ Glutamine and the effects of exhaust... [Can J Physiol Pharmacol. 1998] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/9839078
- Jump up ↑ Vitamin C supplementation reduces the incidence of postrace symptoms of upper-respiratory-tract infection in ultramarathon runners http://www.ajcn.org/content/57/2/170.abstract?ijkey=353d1bf015076ca918c148006e8bdae68eb2859b&keytype2=tf_ipsecsha
- ↑ Jump up to: 17.0 17.1 Peters EM, et al, Vitamin C as effective as combinations of anti-oxidant nutrients in reducing symptoms of upper respiratory tract infection (URTI) in ultramarathon runners
- Jump up ↑ Nutritional modulation of exercise-induced i... [Eur J Clin Nutr. 2007] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/17136044?dopt=Abstract
- Jump up ↑ Jan9 http://faculty.css.edu/tboone2/asep/jan9.htm
- Jump up ↑ Vitamin supplement use may reduce effects of Alzheimer's disease http://www.eurekalert.org/pub_releases/2004-01/jhub-vsu011504.php
- Jump up ↑ Oral administration of the probiotic Lactoba... [Br J Sports Med. 2010] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/18272539
- Jump up ↑ The effect of probiotics on res... [Int J Sport Nutr Exerc Metab. 2007] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/17962710?dopt=Abstract
- Jump up ↑ Allergy in marathon runners and effect of Lactoba... [Respir Med. 2007] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/17196811?dopt=Abstract
- Jump up ↑ Effects of oral supplementation wi... [Biosci Biotechnol Biochem. 2009] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/19352043
- Jump up ↑ Cystine and Theanine Supplementation Restores High-Intensity... : The Journal of Strength & Conditioning Research http://journals.lww.com/nsca-jscr/Abstract/2010/03000/Cystine_and_Theanine_Supplementation_Restores.34.aspx
- Jump up ↑ JC. Kassel, D. King, GK. Spurling, Saline nasal irrigation for acute upper respiratory tract infections., Cochrane Database Syst Rev, issue 3, pages CD006821, 2010, doi 10.1002/14651858.CD006821.pub2, PMID 20238351
