Cryotherapy
Contents
1 The science
I would have like to write this article based on scientific research, but there is remarkably little available. A 2004 analysis of the available research at the time stated "Currently, no authors have assessed the efficacy of ice in the treatment of muscle contusions or strains. Considering that most injuries are muscle strains and contusions, this is a large void in the literature." A 2008 study stated in its conclusion "There is insufficient evidence to suggest that cryotherapy improves clinical outcome in the management of soft tissue injuries"[1][2]. We'll therefore look at some anecdotal, real world experiences and recommendations.
2 Common Recommendations
The general recommendation for ice is to apply it for 20 minutes, then remove it for 20-60 minutes, repeating this cycle several times [3]. The general advice is to avoid applying ice for too long as it can damage the skin. I have found while this approach does help a little, it is not as effective as leaving the ice in place for a much longer period.
3 Longer Applications
Does a longer period make sense? Well, a Study has shown that the time needed to cool a muscle varies with the thickness of the fat surrounding the muscle. To lower the temperature 1 cm into the muscle by 7 degrees C, it takes ~8 minutes of ice for 0-10mm fat, but ~60 mins for 21-30mm fat[4]. This suggests that a simplistic 'apply for 20 minutes' guide is inappropriate; to impact tissue that is an inch deep would require at least an hour. One study[5] applied ice for 30 minutes and recorded the temperature at 1 and 2 cm into the muscle (below the fat layer). The results indicated that the minimum temperature was not reached during the application, but 6 to 9 minutes after the application finished. This suggests that 30 minutes was not sufficient to fully cool the muscle. Other factors to consider:
4 My Approach
My personal approach is to apply ice for much longer; often for hours continuously. I find that this produces much deeper healing and I have never had any problems. However, there are a number of conditions that would make this approach dangerous, such as poor circulation, diabetes or arthritis[8]. You should also be careful about applying ice for prolonged periods at joints such as elbow or ankle; the nerves are closer to the surface. I know some people like to use a compression bandage to hold the ice in place, adding compression to the cooling.
5 Frostbite and skin damage
Damage to cells occurs around -10c/14f[9][10], which is well below the temperature of ice. In fact, the temperature of the skin at were it is in contact with an ice pack is normally about 5c/41f[11]. Animal studies that chilled the skin and underlying fat to between -1c/31f and -7c/19f showed no signs of tissue damage[12].
6 Danger - Avoid Gel Packs and Frozen Vegetables
I use ice in a hefty Ziploc bag rather than gel packs as Gel packs start off too cold, then warm up too quickly. If you use ice, the temperature will remain constant around freezing until all the ice is melted[8]. If you use gel packs, or frozen vegetables, you risk frostbite.
7 Ice, Inflammation and Healing
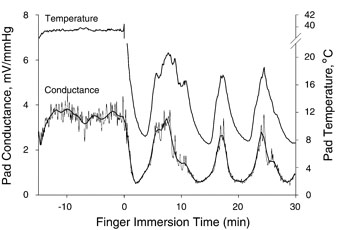
A widely publicized 2010 study[13] has shown that inflammation is necessary for healing, something that has been known for some time[14]. The study did not look at the use of ice for healing, only the role of inflammation itself, so I believe the popular conclusions are flawed. While ice does have some anti-inflammatory properties, ice also increases blood flow (cold induced vasodilatation[15]). This alternating reduction in inflammation and increased blood flow is believed to act as a ‘pump’, speeding up heeling. This cycle typically takes a few minutes, as shown below.
8 See Also
9 References
- ↑ Does Cryotherapy Improve Outcomes With Soft Tissue Injury? http://www.ncbi.nlm.nih.gov/pmc/articles/PMC522152/?tool=pubmed
- ↑ Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? http://www.ncbi.nlm.nih.gov/pubmed/18212134
- ↑ The essential massage companion http://books.google.com/books?id=KXffk6V_ziMC&lpg=PA34&ots=AXhXNofzD9&dq=ice%20%22hunting%20effect%22&pg=PA35#v=onepage&q=ice%20%22hunting%20effect%22&f=false
- ↑ Subcutaneous adipose tissue thickness alters cooling time during cryotherapy http://www.archives-pmr.org/article/PIIS0003999302002423/fulltext
- ↑ 5.0 5.1 Intramuscular temperature response... [J Orthop Sports Phys Ther. 1998] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/9549714
- ↑ http://journals.humankinetics.com/jsr-back-issues/jsrvolume6issue4november/theeffectsofcryotherapyappliedthroughvariousbarriers
- ↑ The Effects Of Ice And Compression Wraps On Intramuscular Temperatures At Various Depths http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317720/
- ↑ 8.0 8.1 Cold Modalities With Different Thermodynamic Properties Produce Different Surface and Intramuscular Temperatures http://www.ncbi.nlm.nih.gov/pubmed/12937469
- ↑ What temperature is lethal for cells? [J Dermatol Surg Oncol. 1979] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/110858
- ↑ Critical temperature for skin necrosis in experi... [Cryobiology. 1982] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/7105779
- ↑ The effect of quantity of ice and size of cont... [Physiotherapy. 2009] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/19627693
- ↑ Cryolipolysis for subcutaneous fat layer red... [Lasers Surg Med. 2009] - PubMed - NCBI http://www.ncbi.nlm.nih.gov/pubmed/20014262
- ↑ Putting ice on injuries could slow healing http://www.telegraph.co.uk/health/healthnews/8087777/Putting-ice-on-injuries-could-slow-healing.html
- ↑ Decreasing Inflammatory Response of Injured Patellar Tendons Results in Increased Collagen Fibril Diameters http://www.pitt.edu/~mechbio/publications/decreasinginflammatory.pdf
- ↑ Reproducibility of the cold-induced vasodilation response in the human finger http://jap.physiology.org/content/98/4/1334.full