Lactate Threshold
Lactate Threshold is a key component of running performance and is a better predictor of race performance than V̇O2max. You can think of Lactate Threshold as reflecting a change from aerobic exercise to anaerobic exercise. Lactate Threshold is often used to determine the correct pace for Tempo Runs, though the science shows such training is ineffective. However, Lactate Threshold provides an excellent way of monitoring the effectiveness of your training and provides an objective estimate of your race pace. Unfortunately, measuring an athlete's Lactate Threshold is time-consuming and expensive, with the gold standard MLSS test requiring three to five 30 minute tests on separate days. All other approaches to measuring an athlete's Lactate Threshold seem deeply flawed. A better approach to your anaerobic threshold is Critical Power.
Contents
- 1 What is Lactate?
- 2 What is the Lactate Threshold?
- 3 Lactate Threshold Training
- 4 The Usefulness of Lactate Threshold
- 5 Lactate Curve
- 6 Determining Your Lactate Threshold
- 7 Factors That May Influence An Athlete's Lactate Threshold
- 8 Aerobic Threshold
- 9 References
1 What is Lactate?
Main article: Lactate
At one time, athletes viewed Lactate as a harmful waste product of anaerobic exercise, but research since the early 2000s has shown that Lactate is an intermediate fuel in the metabolism of carbohydrates. Muscles will burn Lactate in preference to Glucose and will convert Lactate back to Glucose at rest. The level of Lactate in the blood primarily depends on exercise intensity, rather like Heart Rate. Lactate is a fuel source for working muscles, and injecting extra lactate into the blood results in increased lactate metabolism and carbohydrate sparing[1] without impairing performance[2]. Note that Lactate forms Lactic Acid in the blood, and literature uses the terms interchangeably.
2 What is the Lactate Threshold?
The Lactate Threshold (LT) is the point at which the lactate level in your blood will rise even if you keep the work intensity constant. This can be referred to as the Anaerobic Threshold (AT), or the Onset of Blood Lactate Accumulation (OBLA), though the most accurate term is Maximal Lactate Steady State (MLSS). Even within the scientific community terminology is confusing[3]. It is sometimes claimed that the MLSS represents the maximum clearance of Lactate, but this may not be the case[2]. Note that you normally measure Lactate in the bloodstream, so the Lactate level reflects the net of the muscles releasing and absorbing Lactate. Lactate Threshold is important as it is an excellent good predictor of race performance[4][5][6][7][8][9], and may be a better predictor than V̇O2max[10]. You can think of Lactate Threshold as the percentage of VO2max that you can maintain for a protracted time[11]. (It's not clear what the limiting factor is for exercise above the Lactate Threshold[12].)
3 Lactate Threshold Training
Main article: Tempo Runs
There is good evidence that endurance training changes Lactate Threshold. However, the idea that training at threshold intensity, such as Tempo Runs, is particularly effective has no evidence[13]"/>[14], and polarized training is a better approach[15][16]. For trained athletes, Tempo runs are ineffective[17] and may be counterproductive[18][14]. See Tempo Runs for more details. Detraining will reduce your Lactate Threshold[19], and your Lactate levels can be higher at a given intensity after just a few days without training[20], suggesting rapid detraining effects. The improvements in Lactate Threshold pace are largely because of a greater rate of Lactate removal rather than a reduced rate of production[21][22][23][24][25].
4 The Usefulness of Lactate Threshold
One of the primary goals of Lactate Threshold testing has been to determine the correct pace for Tempo Runs. However, even if Tempo training is ineffective, there are two good reasons for knowing your Lactate Threshold. First, monitoring your Lactate Threshold is great for evaluating the effectiveness of a training regime. Second, Lactate Threshold can validate race pace goals. If your Lactate Threshold indicates a much faster race pace than you've been able to achieve, it suggests either a lack of resistance to muscular damage or a lack of mental fortitude. If the Lactate Threshold suggests a race pace that is slower than your target goal, it suggests your goal is wrong and you should aim for a slower finish time. This is especially important in the marathon where hitting the wall is a common issue.
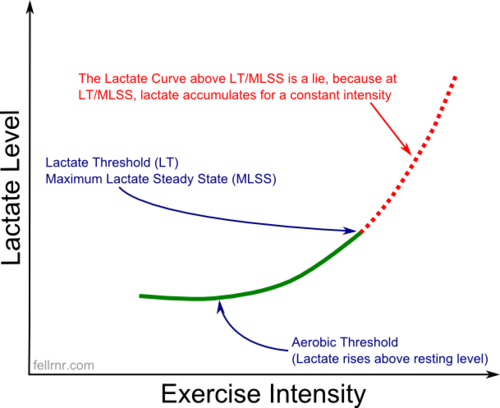
5 Lactate Curve
It is common to plot exercise intensity against the lactate level to produce a blood lactate curve similar to the one below, showing an exponential rise in lactate level with intensity. It's generally accepted that a shift of the curve to the right shows an improved athletic performance[26][27], and training can improve performance because of this shift without a change in aerobic capacity (V̇O2max)[28]. There is some limited evidence from radio-isotope studies in animals that a benefit of endurance training may be in Lactate clearance[24]. Above the Lactate Threshold, the Lactate level is not at a steady-state but rises even though the intensity remains constant, so the typical curve shown below is rather misleading. Some Lactate Curves are plotting Blood Lactate against time during an Incremental Power Test (see below), which is more reasonable but is still misleading.
6 Determining Your Lactate Threshold
There are various ways of determining the Lactate Threshold, each with their problems.
- Critical Power. A better alternative is to ignore Lactate and focus on power output. With Stryd this can be applied to running, though Critical Power tests for runners may have a higher risk for injury. Before Stryd, the approach was to use "Critical Speed" on level ground. See Critical Power for details.
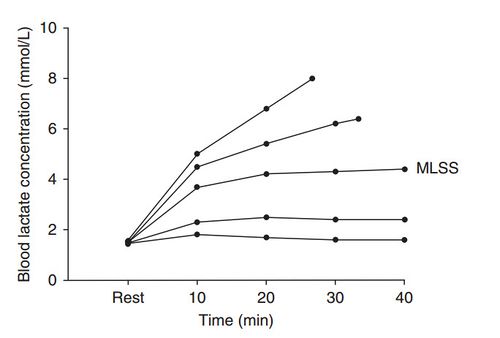
- MLSS. The gold standard test for Lactate Threshold (and the only one that appears to be valid) is to measure Maximal Lactate Steady State (MLSS). The test requires 3 to 5 constant intensity trials of at least 30 minutes' duration, each performed on separate days. Each test is at a different exercise intensity, and the highest intensity that does not have a rise in blood lactate in the last 20 minutes is the MLSS. While this is the best way of determining the Lactate threshold, it's time-consuming and interferes with the athlete's regular training. Even though MLSS is the best approach to determining the Lactate Threshold, there are issues with MLSS and Critical Power is probably a better approach.
- Fixed Blood Lactate Accumulation. A simple approach is to assume that the Lactate Threshold always occurs at the same Lactate level. Sadly, this assumption is wrong, as Lactate Threshold can occur at vastly different levels.
- Lactate Patterns. Some approaches look at the pattern of change in Lactate in an attempt to create a simple test. So far, I've seen little evidence to support any of these approaches.
- Heart Rate Deflection. An indirect way of finding the Lactate Threshold is to look for the Heart Rate Deflection, sometimes called the "Conconi test". This test only requires a heart rate monitor to perform rather than blood draws, so it is much easier than the above approaches. However, the validity of the Conconi test has many issues and seems of dubious value[29]. See Heart Rate Deflection for details.
- Respiratory gasses. Another method for estimating Lactate Threshold is to measure the respiratory gasses[3][30], but given this is impractical for most athletes, it's not covered here.
6.1 Lactate Threshold & Maximal Lactate Steady State
The best approach to determine an athlete's Lactate Threshold is to measure the Maximal Lactate Steady State (MLSS)[31]. The test is several constant load trials of at least 30 minutes' duration on different days at various exercise intensities (between 50–90% V̇O2max. The highest workload that results in an increase of less than 1 mmol/L of lactate between the 10 and 30 minute mark defines the MLSS[32][33][34]. Lactate is typically measured using a blood sample, either using a pinprick or a catheter. Note that MLSS for an individual will vary by sport[35], probably based on the mass of muscle engaged[36][37]. The difficulty of performing this test makes it impractical in most situations. Researchers have raised concerns that even when performed correctly, there are issues with MLSS and suggest that Critical Power is a better approach[38]. The primary issue is that MLSS doesn't truly represent the upper limit of aerobic capacity.
6.2 Lactate Threshold & Incremental Power Test
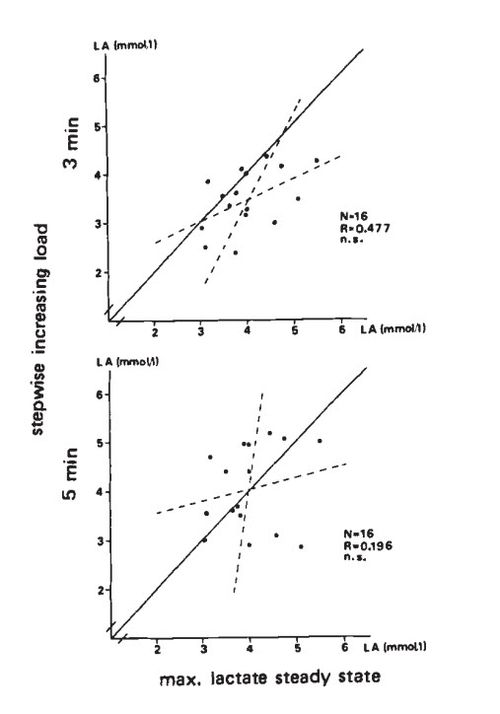
A common approach to determine the Lactate Threshold is the Incremental Power Test. The subject exercises in stages of increasing intensity, with lactate measured at the end of each stage, with stages typically lasting 3 to 10 minutes. However, blood lactate takes 20-30 minutes to stabilize for an intensity[4]. This means that the incremental power test is of limited value[39], with 3 minute stages giving low reproducibility[40], the stage length changing the lactate values[31], and even longer stages lengths of 8 minutes having low reproducibility[41]. The lactate level can drop between the 4th and 12th minute of exercise at a constant intensity[42]. Some have suggested using the lactate value measured as a sign of the prior stage's intensity, as it takes over 3 minutes for lactate to stabilize[43], but this rather arbitrary approach might be a guideline[6]. For running, it is common to pause the exercise for 30 seconds to take a blood sample. These breaks only make a non-significant difference to the testing, though the slight difference tends to be greater at higher intensities[44].
6.3 Lactate Threshold & Fixed Blood Lactate Accumulation
Because MLSS is time consuming and expensive, a shortcut is often used to estimate MLSS by assuming that it occurs at a fixed Lactate Level (Fixed Blood Lactate Accumulation, or FBLA)[33], unusually 4.0 mmol/l[45] though sometimes 3.5 mmol/l[46][47]. However, while the MLSS may average around 4.0 mmol/l[47], there are significant differences for individuals[48], with variations between 3.0 and 5.5 in small sample sizes[45] and has been shown to have a range as wide as 2.0 to 10.0 mmol/l[31][49]. This approach also typically uses a blood test, but in some sports (like running), the athlete has to pause to have a pinprick blood sample taken, further confusing the test[45]. The term "Individual Anaerobic Threshold" (IAT) has been used to emphasize that the Lactate Threshold is specific to each individual rather than using a Fixed Blood Lactate Accumulation, though this can refer to a specific protocol for estimating MLSS[49]. The Fixed Blood Lactate Accumulation is sometimes called "Onset of Blood Lactate Accumulation" (OBLA)[48], a particularly misleading term in this context.
6.4 Lactate Threshold Estimation From Lactate Patterns
There have been several approaches to determining MLSS without the difficulty of the full protocol[50][51][52][53][32], but their validity is limited[54][33][55][56]. These approaches generally look for some pattern in the change of Lactate level.
- For example, one approach called the "Lactate Minimum Speed Test" (LMST) uses an initial sprint to elevate blood lactate followed by an incremental power test[57][58][59]. However, the effectiveness of the LMST is profoundly impacted by the starting speed of the incremental portion of the test[60]and so the results may be coincidence[61]. This is not entirely surprising given the initial sprint phase disrupts the metabolism[61].
- Some trivial approaches have been tried, such as looking for a 1 mmol/l increase followed by another 1 mmol/l increase[62]. So for an athlete performing an incremental load test with Lactate readings of 1.7, 2.3, 2.6, 3.7, & 5.6 the conclusion would be their Lactate Threshold is 3.7 (3.7 is over 1.0 over 2.6 and followed by another increment of over 1.0.) However, given that most portable Lactate meters have a Typical Error of 0.4-1.0 mmol/l[63], a fractional error in the reading gives a different result. In the previous example, if the 2.6 reading was 2.8, then the Lactate Threshold would jump from 3.7 to 5.6.
- Part of the problem with these approaches may be that MLSS may not represent the point of maximum lactate clearance[37], as injecting additional lactate into the blood of athletes exercising above MLSS did not significantly increase lactate levels[2].
- Some of the tests could be "p-hacking", where the study looks at a sufficiently large number of variables that some correlation occurs randomly[64].
- One approach that looks promising uses three tests to estimate MLSS[65]. First, a standard incremental test is used to give a rough estimate of MLSS. Then two 30 minute tests are performed, one above and one below the rough estimate of MLSS. The relative difference in the rise between the two tests is then used to estimate the crossover point. For instance, assume running at 7:00 min/mile produced a blood lactate level that fell from 4 mmol/l at 5 min to 3 mmol/l at 20 min, a 1 mmol/l drop. Then a run at In the run at 6:20 min/mile the blood lactate rose from 4.0 mmol/l at 5 min to 6.5 mmol/l at 20 min, a 1.5 mmol/l rise. The interception point would then be about an MLSS pace of 6:26 min/mile. This is not much less effort than the full MLSS test, but it is an improvement.
6.5 Lactate Threshold and Near-Infrared Spectroscopy
A promising technology for measuring Lactate Threshold is Near-infrared spectroscopy (NIRS) which shines infrared light into the skin above an active muscle and measures the reflected light. NIRS measures the oxygen saturation in the capillaries of the muscle and has the potential to test for Lactate Threshold with no blood sampling. Because NIRS can monitor continually, it may be able to determine the Lactate Threshold during an incremental test rather than requiring the multiple tests of MLSS.
6.5.1 Introduction to NIRS and SmO2
Near-infrared spectroscopy (NIRS) has been shown to measure the oxygen saturation of blood in muscle (SmO2) or other body tissues (StO2)[66][67][68]. (This works on similar principles to a Pulse Oximeter.) Medical NIRS systems for monitoring StO2 use Infrared LED or Lasers at 2, 3, or 4 frequencies[69]. SmO2 reflects the balance of oxygen delivery and consumption during exercise[70]. There are some initial indications that relative SmO2 may reflect changes in performance capacity[71]. There is generally a four-phase response of smo2 during incremental exercise from rest to maximum intensity and the following recovery[72]:
- An initial increase in SmO2 above resting levels to supply the now active muscles. (This may be due to increased blood flow[73], but computer models do not support this[74].)
- SmO2 decreases linearly or exponentially with increasing intensity, followed by a leveling off as the subject approaches maximum intensity. There is some evidence of a breakpoint where the rate of decline increases (see below).
- During the first 1-2 minutes of recovery, there is a rapid increase in SmO2 which usually exceeds resting levels.
- SmO2 then declines to resting levels over a further few minutes.
Skin should not impact SmO2 readings more than 5%[75], but surface fat can interfere with smo2[76][77][78][79]. Because the penetration depth of NIRS is about 50-60% of the distance between the emitter and receiver, the site must be selected so that the fat layer is much thinner than this depth[80]. (It's been suggested that SmO2 is probably only viable in lean individuals.)
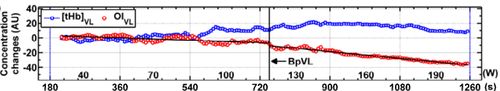
6.5.2 SmO2 Breakpoint
As the intensity increases during incremental exercise SmO2 will remain constant or decline, with the rate of decline being greater near the Lactate Threshold[72][80][81]. This has led to several studies using the concept of an SmO2 "breakpoint"[82]. This breakpoint is a change in the slope of the line plotting SmO2 against work intensity in an incremental intensity test. This increase in the rate of desaturation can either be visually determined or based on bilinear regression. (The bilinear regression iterates over different combinations of two regression lines to find the lowest sum of squares of the residuals. I could not find the details of the constraints placed on this approach.)
Another approach used by[83] was defined as the workload immediately before a drop of 15% that lead to a continuous decline in SmO2. This is shown in the image below, showing a recording with and without a defined breakpoint.
6.5.3 SmO2 and Lactate Threshold
Several studies have looked at the relationship between SmO2 and Lactate or Lactate Threshold
- A study of five mountain climbers found a relationship between the "point of inflection of lactate" and the SmO2 breakpoint during an incremental cycling test[82]. The definition they were using for the inflection of lactate was a blood lactate reading that is more than 0.5 below the subsequent value, with typical lactate levels below 2 mmol/l. This is closer to the "aerobic threshold" concept than the typical Lactate Threshold. The study did not find any correlation between the SmO2 breakpoint and the 4 mmol/L blood lactate level. The breakpoint was determined from bi-linear regression.
- A study of 40 sedentary undergraduates showed a correlation between SmO2 returning to resting levels and Ventilatory Threshold (VT) in 65% of subjects during an incremental cycling test[73]. While the text refers to Lactate Threshold as the point at which Lactate rises above resting levels (aerobic threshold) the method used to determine VT appears to be the anaerobic threshold. This study did not use the breakpoint mentioned above, but the point where the SmO2 drops below the level detected at rest.
- A study of 11 subjects of varying fitness levels showed a correlation between SmO2 breakpoint determined visually and Ventilatory Threshold (VT) during an incremental cycling test[72].
- A comparison between 12 healthy subjects and 7 suffering from chronic heart failure (CHF) showed a correlation between the SmO2 breakpoint and Ventilatory Threshold (VT) during an incremental cycling test[84].
- A 2012 study compared the results from NIRS on the calf (Gastrocnemius Lateralis) and quads (Vastus Lateralis) in 31 active but not highly trained college students during an incremental cycling test[85]. The study found a correlation between Lactate Threshold (determined from the log-log method[86]) and the SmO2 breakpoint (determined from bi-linear regression) in both locations, but the quads corresponded better. (I suspect the results from running could be quite different.)
- A 2009 study used MLSS (the gold standard for Lactate Threshold) with running to test NIRS[83]. The 16 athletes performed between 2 and 5 tests of 30 minutes each to determine MLSS, separated by at least 48 hours each. The subjects then performed an incremental treadmill test using 6-minute stages with the 4th stage at the pace they estimated they could maintain for an hour (around Lactate Threshold). The first 3 stages where then 0.66, 0.44, & 0.22 meter/second slower, and the subsequent stages were 0.22 meters/second faster each time. SmO2 breakpoint was defined as the workload immediately before a drop of 15% that lead to a continuous decline in SmO2. A Lactate breakpoint was also determined based on the incremental test using the workload before an increase of 1 mmol/l as the criteria. Both the SmO2 and the Lactate breakpoint were determined visually. Of the 16 subjects, 1 did not reach MLSS, 2 did not have both a SmO2 breakpoint or a Lactate breakpoint (based on the criteria used) and 1 had neither. The study found that SmO2 is as effective as Lactate breakpoint tests for determining true Lactate Threshold (MLSS). The table below shows the values for each of 12 subjects, with the paces shown as KPH, then min/mile, then the error as a percentage. This shows that while smo2 is as good as the lactate breakpoint, the individual differences from MLSS are not insignificant. For instance, subject 5 had an MLSS of 6:21, but an SmO2 breakpoint of 6:57 and a lactate breakpoint of 6:59, which is a big difference.
| Subject | MLSS | SmO2 | Lb | MLSS | SmO2 | Lb | SmO2 err | Lb err |
|---|---|---|---|---|---|---|---|---|
| 1 | 13.5 | 12.9 | 13.7 | 7:09 | 7:29 | 7:03 | 4.4% | -1.5% |
| 2 | 14.3 | 14.2 | 13.4 | 6:45 | 6:48 | 7:12 | 0.7% | 6.3% |
| 3 | 9 | 9.5 | 9.5 | 10:44 | 10:10 | 10:10 | -5.6% | -5.6% |
| 4 | 13.4 | 12.9 | 12.9 | 7:12 | 7:29 | 7:29 | 3.7% | 3.7% |
| 5 | 15.2 | 13.9 | 13.8 | 6:21 | 6:57 | 6:59 | 8.6% | 9.2% |
| 6 | 12.9 | 12.7 | 13.5 | 7:29 | 7:36 | 7:09 | 1.6% | -4.7% |
| 7 | 15.4 | 14.5 | 15.3 | 6:16 | 6:40 | 6:19 | 5.8% | 0.6% |
| 8 | 11.5 | 11.7 | 10.9 | 8:24 | 8:15 | 8:52 | -1.7% | 5.2% |
| 9 | 10.8 | 10.9 | 10.8 | 8:56 | 8:52 | 8:56 | -0.9% | 0.0% |
| 10 | 14.2 | 14.2 | 13.2 | 6:48 | 6:48 | 7:19 | 0.0% | 7.0% |
| 11 | 11.6 | 12.2 | 12.2 | 8:19 | 7:55 | 7:55 | -5.2% | -5.2% |
| 12 | 14.8 | 14.6 | 13.8 | 6:31 | 6:37 | 6:59 | 1.4% | 6.8% |
| Mean | 13.05 | 12.85 | 12.75 | |||||
| SD | 1.88 | 1.51 | 1.55 |
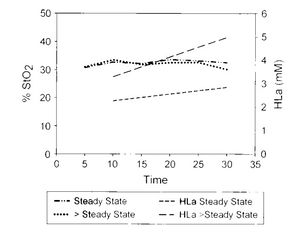
6.5.4 SmO2 and MLSS
Sadly, there does not appear to be a difference in SmO2 during an MLSS test above and below the MLSS threshold pace[83]. If running above the MLSS threshold pace does not result in a drop in smo2, then the ability to use SmO2 for finding threshold seems rather dubious.
6.5.5 Thoughts on SmO2 and Lactate Threshold
I think the available research shows that NIRS and SmO2 might hold promise for simplifying the measurement of Lactate Threshold. However, the research is at a fairly early stage, with only one study using the gold standard of MLSS, and the results are mixed at best. In some ways, I feel the MLSS test above shows that SmO2 is a poor option for evaluating an athlete's Lactate Threshold, but perhaps most existing approaches other than a full MLSS test are equally flawed. Currently, there are two consumer products available; BSX and Moxy. BSX is a fully automated approach to analyzing the data and estimating Lactate Threshold, whereas the Moxy is intended to provide the end-user with the underlying data to evaluate. (BSX is being discontinued.)
7 Factors That May Influence An Athlete's Lactate Threshold
There are a few factors that may change the Lactate Threshold (other than training)
- Because lactate is produced from the metabolism of carbohydrate, a reduction in carbohydrate intake (or Glycogen depletion) will shift the lactate curve to the right[87][88][89][90].
- It's not clear if Delayed Onset Muscle Soreness changes the lactate curve as there are reports that it does[91] and reports that it does not[92].
- Lactate Threshold will vary by sport, probably based on the mass of muscle engaged[36], or because the inactive muscles consume more lactate as the concentration rises[43]. MLSS may also vary with environmental conditions, with a lower lactate levels at MLSS in hotter conditions[93].
8 Aerobic Threshold
There is a related concept called "Aerobic Threshold" that is generally used to mean the exercise intensity at which Lactate levels rise above resting baselines[31]. This threshold is believed to be the upper limit of nearly exclusive use of aerobic metabolism that can be sustained for many hours. Intensities just above the aerobic threshold can be maintained for prolonged periods (~4 hours)[94]. This aerobic threshold can be hard to determine in untrained subjects as it occurs at very low intensities[95]. Unfortunately, the term "Lactate Threshold" is sometimes used to mean this point where lactate rises above resting levels[88].
9 References
- ↑ Benjamin F. Miller, Jill A. Fattor, Kevin A. Jacobs, Michael A. Horning, Franco Navazio, Michael I. Lindinger, George A. Brooks, Lactate and glucose interactions during rest and exercise in men: effect of exogenous lactate infusion, The Journal of Physiology, volume 544, issue 3, 2002, pages 963–975, ISSN 00223751, doi 10.1113/jphysiol.2002.027128
- ↑ 2.0 2.1 2.2 Darren Ellis, Catherine Simmons, Benjamin F. Miller, Sodium lactate infusion during a cycling time-trial does not increase lactate concentration or decrease performance, European Journal of Sport Science, volume 9, issue 6, 2009, pages 367–374, ISSN 1746-1391, doi 10.1080/17461390903009158
- ↑ 3.0 3.1 RK. Binder, M. Wonisch, U. Corra, A. Cohen-Solal, L. Vanhees, H. Saner, JP. Schmid, Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing., Eur J Cardiovasc Prev Rehabil, volume 15, issue 6, pages 726-34, Dec 2008, doi 10.1097/HJR.0b013e328304fed4, PMID 19050438
- ↑ 4.0 4.1 LV. Billat, Use of blood lactate measurements for prediction of exercise performance and for control of training. Recommendations for long-distance running., Sports Med, volume 22, issue 3, pages 157-75, Sep 1996, PMID 8883213
- ↑ GS. Palmer, LB. Borghouts, TD. Noakes, JA. Hawley, Metabolic and performance responses to constant-load vs. variable-intensity exercise in trained cyclists., J Appl Physiol (1985), volume 87, issue 3, pages 1186-96, Sep 1999, PMID 10484594
- ↑ 6.0 6.1 C. Baldari, L. Guidetti, A simple method for individual anaerobic threshold as predictor of max lactate steady state., Med Sci Sports Exerc, volume 32, issue 10, pages 1798-802, Oct 2000, PMID 11039656
- ↑ AM. Jones, H. Carter, The effect of endurance training on parameters of aerobic fitness., Sports Med, volume 29, issue 6, pages 373-86, Jun 2000, PMID 10870864
- ↑ M. Lehmann, A. Berg, R. Kapp, T. Wessinghage, J. Keul, Correlations between laboratory testing and distance running performance in marathoners of similar performance ability., Int J Sports Med, volume 4, issue 4, pages 226-30, Nov 1983, doi 10.1055/s-2008-1026039, PMID 6654546
- ↑ K. Tanaka, Y. Matsuura, Marathon performance, anaerobic threshold, and onset of blood lactate accumulation., J Appl Physiol Respir Environ Exerc Physiol, volume 57, issue 3, pages 640-3, Sep 1984, PMID 6490453
- ↑ WK. Allen, DR. Seals, BF. Hurley, AA. Ehsani, JM. Hagberg, Lactate threshold and distance-running performance in young and older endurance athletes., J Appl Physiol (1985), volume 58, issue 4, pages 1281-4, Apr 1985, PMID 3988681
- ↑ DL. Costill, H. Thomason, E. Roberts, Fractional utilization of the aerobic capacity during distance running., Med Sci Sports, volume 5, issue 4, pages 248-52, 1973, PMID 4774203
- ↑ B. Baron, TD. Noakes, J. Dekerle, F. Moullan, S. Robin, R. Matran, P. Pelayo, Why does exercise terminate at the maximal lactate steady state intensity?, Br J Sports Med, volume 42, issue 10, pages 828-33, Oct 2008, doi 10.1136/bjsm.2007.040444, PMID 18070803
- ↑ R. Beneke, RM. Leithäuser, O. Ochentel, Blood lactate diagnostics in exercise testing and training., Int J Sports Physiol Perform, volume 6, issue 1, pages 8-24, Mar 2011, PMID 21487146
- ↑ 14.0 14.1 A. Guellich, S. Seiler, Lactate profile changes in relation to training characteristics in junior elite cyclists., Int J Sports Physiol Perform, volume 5, issue 3, pages 316-27, Sep 2010, PMID 20861522
- ↑ Thomas Stöggl, Billy Sperlich, Polarized training has greater impact on key endurance variables than threshold, high intensity, or high volume training, Frontiers in Physiology, volume 5, 2014, ISSN 1664-042X, doi 10.3389/fphys.2014.00033
- ↑ I. Muñoz, S. Seiler, J. Bautista, J. España, E. Larumbe, J. Esteve-Lanao, Does polarized training improve performance in recreational runners?, Int J Sports Physiol Perform, volume 9, issue 2, pages 265-72, Mar 2014, doi 10.1123/ijspp.2012-0350, PMID 23752040
- ↑ BR. Londeree, Effect of training on lactate/ventilatory thresholds: a meta-analysis., Med Sci Sports Exerc, volume 29, issue 6, pages 837-43, Jun 1997, PMID 9219214
- ↑ F. Evertsen, JI. Medbø, A. Bonen, Effect of training intensity on muscle lactate transporters and lactate threshold of cross-country skiers., Acta Physiol Scand, volume 173, issue 2, pages 195-205, Oct 2001, doi 10.1046/j.1365-201X.2001.00871.x, PMID 11683677
- ↑ EF. Coyle, WH. Martin, SA. Bloomfield, OH. Lowry, JO. Holloszy, Effects of detraining on responses to submaximal exercise., J Appl Physiol (1985), volume 59, issue 3, pages 853-9, Sep 1985, PMID 3902770
- ↑ I. Mujika, S. Padilla, Cardiorespiratory and metabolic characteristics of detraining in humans., Med Sci Sports Exerc, volume 33, issue 3, pages 413-21, Mar 2001, PMID 11252068
- ↑ SM. Phillips, HJ. Green, MA. Tarnopolsky, SM. Grant, Increased clearance of lactate after short-term training in men., J Appl Physiol (1985), volume 79, issue 6, pages 1862-9, Dec 1995, PMID 8847245
- ↑ HS. MacRae, SC. Dennis, AN. Bosch, TD. Noakes, Effects of training on lactate production and removal during progressive exercise in humans., J Appl Physiol (1985), volume 72, issue 5, pages 1649-56, May 1992, PMID 1601768
- ↑ CM. Donovan, MJ. Pagliassotti, Endurance training enhances lactate clearance during hyperlactatemia., Am J Physiol, volume 257, issue 5 Pt 1, pages E782-9, Nov 1989, PMID 2512815
- ↑ 24.0 24.1 CM. Donovan, GA. Brooks, Endurance training affects lactate clearance, not lactate production., Am J Physiol, volume 244, issue 1, pages E83-92, Jan 1983, PMID 6401405
- ↑ BC. Bergman, EE. Wolfel, GE. Butterfield, GD. Lopaschuk, GA. Casazza, MA. Horning, GA. Brooks, Active muscle and whole body lactate kinetics after endurance training in men., J Appl Physiol (1985), volume 87, issue 5, pages 1684-96, Nov 1999, PMID 10562610
- ↑ L. Bosquet, L. Léger, P. Legros, Methods to determine aerobic endurance., Sports Med, volume 32, issue 11, pages 675-700, 2002, PMID 12196030
- ↑ T. Yoshida, M. Udo, M. Chida, M. Ichioka, K. Makiguchi, T. Yamaguchi, Specificity of physiological adaptation to endurance training in distance runners and competitive walkers., Eur J Appl Physiol Occup Physiol, volume 61, issue 3-4, pages 197-201, 1990, PMID 2282901
- ↑ EO. Acevedo, AH. Goldfarb, Increased training intensity effects on plasma lactate, ventilatory threshold, and endurance., Med Sci Sports Exerc, volume 21, issue 5, pages 563-8, Oct 1989, PMID 2607946
- ↑ I Cook, Was the Conconi test validated by sporting success, expert opinion or good science?, South African Journal for Research in Sport, Physical Education and Recreation, volume 33, issue 1, 2011, ISSN 0379-9069, doi 10.4314/sajrs.v33i1.65483
- ↑ D. Laplaud, M. Guinot, A. Favre-Juvin, P. Flore, Maximal lactate steady state determination with a single incremental test exercise., Eur J Appl Physiol, volume 96, issue 4, pages 446-52, Mar 2006, doi 10.1007/s00421-005-0086-4, PMID 16341873
- ↑ 31.0 31.1 31.2 31.3 O. Faude, W. Kindermann, T. Meyer, Lactate threshold concepts: how valid are they?, Sports Med, volume 39, issue 6, pages 469-90, 2009, PMID 19453206
- ↑ 32.0 32.1 A. Urhausen, B. Coen, B. Weiler, W. Kindermann, Individual anaerobic threshold and maximum lactate steady state., Int J Sports Med, volume 14, issue 3, pages 134-9, Apr 1993, doi 10.1055/s-2007-1021157, PMID 8509241
- ↑ 33.0 33.1 33.2 Kristopher Mendes De Souza, Talita Grossl, Rubens José Babel Junior, Ricardo Dantas De Lucas, Vitor Pereira Costa, Luiz Guilherme Antonacci Guglielmo, Máximo estado estável de lactato estimado por diferentes métodos de determinação, Revista Brasileira de Cineantropometria e Desempenho Humano, volume 14, issue 3, 2012, ISSN 1980-0037, doi 10.5007/1980-0037.2012v14n3p264
- ↑ R. Beneke, Methodological aspects of maximal lactate steady state-implications for performance testing., Eur J Appl Physiol, volume 89, issue 1, pages 95-9, Mar 2003, doi 10.1007/s00421-002-0783-1, PMID 12627312
- ↑ TR. Figueira, F. Caputo, JG. Pelarigo, BS. Denadai, Influence of exercise mode and maximal lactate-steady-state concentration on the validity of OBLA to predict maximal lactate-steady-state in active individuals., J Sci Med Sport, volume 11, issue 3, pages 280-6, Jun 2008, doi 10.1016/j.jsams.2007.02.016, PMID 17553745
- ↑ 36.0 36.1 R. Beneke, SP. von Duvillard, Determination of maximal lactate steady state response in selected sports events., Med Sci Sports Exerc, volume 28, issue 2, pages 241-6, Feb 1996, PMID 8775160
- ↑ 37.0 37.1 R. Beneke, Maximal lactate steady state concentration (MLSS): experimental and modelling approaches., Eur J Appl Physiol, volume 88, issue 4-5, pages 361-9, Jan 2003, doi 10.1007/s00421-002-0713-2, PMID 12527964
- ↑ Andrew M. Jones, Mark Burnley, Matthew I. Black, David C. Poole, Anni Vanhatalo, The maximal metabolic steady state: redefining the 'gold standard', Physiological Reports, volume 7, issue 10, 2019, pages e14098, ISSN 2051-817X, doi 10.14814/phy2.14098
- ↑ P. Foxdal, A. Sjödin, B. Sjödin, Comparison of blood lactate concentrations obtained during incremental and constant intensity exercise., Int J Sports Med, volume 17, issue 5, pages 360-5, Jul 1996, doi 10.1055/s-2007-972861, PMID 8858408
- ↑ RH. Morton, SR. Stannard, B. Kay, Low reproducibility of many lactate markers during incremental cycle exercise., Br J Sports Med, volume 46, issue 1, pages 64-9, Jan 2012, doi 10.1136/bjsm.2010.076380, PMID 21343140
- ↑ JP. Gavin, ME. Willems, SD. Myers, Reproducibility of lactate markers during 4 and 8 min stage incremental running: a pilot study., J Sci Med Sport, volume 17, issue 6, pages 635-9, Nov 2014, doi 10.1016/j.jsams.2013.08.006, PMID 24028777
- ↑ M. Rieu, J. Miladi, A. Ferry, A. Duvallet, Blood lactate during submaximal exercises, European Journal of Applied Physiology and Occupational Physiology, volume 59, issue 1-2, 1989, pages 73–79, ISSN 0301-5548, doi 10.1007/BF02396583
- ↑ 43.0 43.1 CJ. Orok, RL. Hughson, HJ. Green, JA. Thomson, Blood lactate responses in incremental exercise as predictors of constant load performance., Eur J Appl Physiol Occup Physiol, volume 59, issue 4, pages 262-7, 1989, PMID 2583172
- ↑ L. Gullstrand, B. Sjüdin, J. Svedenhag, Blood sampling during continuous running and 30-second intervals on a treadmill, Scandinavian Journal of Medicine & Science in Sports, volume 4, issue 4, 2007, pages 239–242, ISSN 09057188, doi 10.1111/j.1600-0838.1994.tb00434.x
- ↑ 45.0 45.1 45.2 45.3 H. Heck, A. Mader, G. Hess, S. Mücke, R. Müller, W. Hollmann, Justification of the 4-mmol/l lactate threshold., Int J Sports Med, volume 6, issue 3, pages 117-30, Jun 1985, doi 10.1055/s-2008-1025824, PMID 4030186
- ↑ B.S. Denadai, T.R. Figueira, O.R.P. Favaro, M. Gonçalves, Effect of the aerobic capacity on the validity of the anaerobic threshold for determination of the maximal lactate steady state in cycling, Brazilian Journal of Medical and Biological Research, volume 37, issue 10, 2004, pages 1551–1556, ISSN 1678-4510, doi 10.1590/S0100-879X2004001000015
- ↑ 47.0 47.1 BS. Denadai, EB. Gomide, CC. Greco, The relationship between onset of blood lactate accumulation, critical velocity, and maximal lactate steady state in soccer players., J Strength Cond Res, volume 19, issue 2, pages 364-8, May 2005, doi [364:TRBOOB2.0.CO;2 10.1519/1533-4287(2005)19[364:TRBOOB]2.0.CO;2], PMID 15903376
- ↑ 48.0 48.1 Mamen, Asgeir. "Estimating the Maximal Lactate Steady State Power from an Incremental Test Using Lactate Pro (R) LP1710." International Journal of Applied sports sciences (IJASS) 21.1 (2009): 74-85.
- ↑ 49.0 49.1 H. Stegmann, W. Kindermann, A. Schnabel, Lactate kinetics and individual anaerobic threshold., Int J Sports Med, volume 2, issue 3, pages 160-5, Aug 1981, doi 10.1055/s-2008-1034604, PMID 7333753
- ↑ CR. Harnish, TC. Swensen, RR. Pate, Methods for estimating the maximal lactate steady state in trained cyclists., Med Sci Sports Exerc, volume 33, issue 6, pages 1052-5, Jun 2001, PMID 11404673
- ↑ AS. Palmer, JA. Potteiger, KL. Nau, RJ. Tong, A 1-day maximal lactate steady-state assessment protocol for trained runners., Med Sci Sports Exerc, volume 31, issue 9, pages 1336-41, Sep 1999, PMID 10487377
- ↑ U. Tegtbur, MW. Busse, KM. Braumann, Estimation of an individual equilibrium between lactate production and catabolism during exercise., Med Sci Sports Exerc, volume 25, issue 5, pages 620-7, May 1993, PMID 8492691
- ↑ HH. Dickhuth, L. Yin, A. Niess, K. Röcker, F. Mayer, HC. Heitkamp, T. Horstmann, Ventilatory, lactate-derived and catecholamine thresholds during incremental treadmill running: relationship and reproducibility., Int J Sports Med, volume 20, issue 2, pages 122-7, Feb 1999, doi 10.1055/s-2007-971105, PMID 10190774
- ↑ AE. Kilding, AM. Jones, Validity of a single-visit protocol to estimate the maximum lactate steady state., Med Sci Sports Exerc, volume 37, issue 10, pages 1734-40, Oct 2005, PMID 16260974
- ↑ R. Beneke, Anaerobic threshold, individual anaerobic threshold, and maximal lactate steady state in rowing., Med Sci Sports Exerc, volume 27, issue 6, pages 863-7, Jun 1995, PMID 7658947
- ↑ AM. Jones, JH. Doust, The validity of the lactate minimum test for determination of the maximal lactate steady state., Med Sci Sports Exerc, volume 30, issue 8, pages 1304-13, Aug 1998, PMID 9710874
- ↑ Rafael da Costa Sotero, Emerson Pardono, Carmen Sílvia Grubert Campbell, Herbert Gustavo Simões, Indirect Assessment of Lactate Minimum and Maximal Blood Lactate Steady-State Intensity for Physically Active Individuals, Journal of Strength and Conditioning Research, volume 23, issue 3, 2009, pages 847–853, ISSN 1064-8011, doi 10.1519/JSC.0b013e318196b609
- ↑ RC. Sotero, E. Pardono, R. Landwehr, CS. Campbell, HG. Simoes, Blood glucose minimum predicts maximal lactate steady state on running., Int J Sports Med, volume 30, issue 9, pages 643-6, Sep 2009, doi 10.1055/s-0029-1220729, PMID 19569005
- ↑ Willian Eiji Miyagi, Jorge Vieira de Mello Leite, Alessandro Moura Zagatto, Influência da seleção dos estágios incrementais sobre a intensidade de lactato mínimo: estudo piloto, Revista Brasileira de Cineantropometria e Desempenho Humano, volume 15, issue 6, 2013, ISSN 1980-0037, doi 10.5007/1980-0037.2013v15n6p715
- ↑ H. Carter, AM. Jones, JH. Doust, Effect of incremental test protocol on the lactate minimum speed., Med Sci Sports Exerc, volume 31, issue 6, pages 837-45, Jun 1999, PMID 10378911
- ↑ 61.0 61.1 H. Carter, AM. Jones, JH. Doust, Changes in blood lactate and pyruvate concentrations and the lactate-to-pyruvate ratio during the lactate minimum speed test., J Sports Sci, volume 18, issue 3, pages 213-25, Mar 2000, doi 10.1080/026404100365117, PMID 10737272
- ↑ The Performance Benefits of Lactate Threshold Testing and Training - CTS, http://trainright.com/the-performance-benefits-of-lactate-threshold-testing-and-training/, Accessed on 22 August 2015
- ↑ RK. Tanner, KL. Fuller, ML. Ross, Evaluation of three portable blood lactate analysers: Lactate Pro, Lactate Scout and Lactate Plus., Eur J Appl Physiol, volume 109, issue 3, pages 551-9, Jun 2010, doi 10.1007/s00421-010-1379-9, PMID 20145946
- ↑ Megan L. Head, Luke Holman, Rob Lanfear, Andrew T. Kahn, Michael D. Jennions, The Extent and Consequences of P-Hacking in Science, PLOS Biology, volume 13, issue 3, 2015, pages e1002106, ISSN 1545-7885, doi 10.1371/journal.pbio.1002106
- ↑ V. Billat, F. Dalmay, MT. Antonini, AP. Chassain, A method for determining the maximal steady state of blood lactate concentration from two levels of submaximal exercise., Eur J Appl Physiol Occup Physiol, volume 69, issue 3, pages 196-202, 1994, PMID 8001529
- ↑ KJ. Kek, R. Kibe, M. Niwayama, N. Kudo, K. Yamamoto, Optical imaging instrument for muscle oxygenation based on spatially resolved spectroscopy., Opt Express, volume 16, issue 22, pages 18173-87, Oct 2008, PMID 18958095
- ↑ A. Torricelli, V. Quaresima, A. Pifferi, G. Biscotti, L. Spinelli, P. Taroni, M. Ferrari, R. Cubeddu, Mapping of calf muscle oxygenation and haemoglobin content during dynamic plantar flexion exercise by multi-channel time-resolved near-infrared spectroscopy., Phys Med Biol, volume 49, issue 5, pages 685-99, Mar 2004, PMID 15070196
- ↑ DM. Mancini, L. Bolinger, H. Li, K. Kendrick, B. Chance, JR. Wilson, Validation of near-infrared spectroscopy in humans., J Appl Physiol (1985), volume 77, issue 6, pages 2740-7, Dec 1994, PMID 7896615
- ↑ S. Hyttel-Sorensen, LC. Sorensen, J. Riera, G. Greisen, Tissue oximetry: a comparison of mean values of regional tissue saturation, reproducibility and dynamic range of four NIRS-instruments on the human forearm., Biomed Opt Express, volume 2, issue 11, pages 3047-57, Nov 2011, doi 10.1364/BOE.2.003047, PMID 22076266
- ↑ B. Chance, MT. Dait, C. Zhang, T. Hamaoka, F. Hagerman, Recovery from exercise-induced desaturation in the quadriceps muscles of elite competitive rowers., Am J Physiol, volume 262, issue 3 Pt 1, pages C766-75, Mar 1992, PMID 1312785
- ↑ JP. Neary, DC. McKenzie, YN. Bhambhani, Muscle oxygenation trends after tapering in trained cyclists., Dyn Med, volume 4, issue 1, pages 4, Mar 2005, doi 10.1186/1476-5918-4-4, PMID 15790400
- ↑ 72.0 72.1 72.2 R. Belardinelli, TJ. Barstow, J. Porszasz, K. Wasserman, Changes in skeletal muscle oxygenation during incremental exercise measured with near infrared spectroscopy., Eur J Appl Physiol Occup Physiol, volume 70, issue 6, pages 487-92, 1995, PMID 7556120
- ↑ 73.0 73.1 YN. Bhambhani, SM. Buckley, T. Susaki, Detection of ventilatory threshold using near infrared spectroscopy in men and women., Med Sci Sports Exerc, volume 29, issue 3, pages 402-9, Mar 1997, PMID 9139181
- ↑ AJ. Fuglevand, SS. Segal, Simulation of motor unit recruitment and microvascular unit perfusion: spatial considerations., J Appl Physiol (1985), volume 83, issue 4, pages 1223-34, Oct 1997, PMID 9338432
- ↑ NB. Hampson, CA. Piantadosi, Near infrared monitoring of human skeletal muscle oxygenation during forearm ischemia., J Appl Physiol (1985), volume 64, issue 6, pages 2449-57, Jun 1988, PMID 3403428
- ↑ MC. van Beekvelt, MS. Borghuis, BG. van Engelen, RA. Wevers, WN. Colier, Adipose tissue thickness affects in vivo quantitative near-IR spectroscopy in human skeletal muscle., Clin Sci (Lond), volume 101, issue 1, pages 21-8, Jul 2001, PMID 11410110
- ↑ Sachiko Homma, Influence of adipose tissue thickness on near infrared spectroscopic signal in the measurement of human muscle, Journal of Biomedical Optics, volume 1, issue 4, 1996, pages 418, ISSN 10833668, doi 10.1117/12.252417
- ↑ David A. Benaron, Kenichi Matsushita, Sachiko Homma, Eiji Okada, Britton Chance, Marco Ferrari, <title>Influence of adipose tissue on muscle oxygenation measurement with an NIRS instrument</title>, volume 3194, 1998, pages 159–165, ISSN 0277786X, doi 10.1117/12.301048
- ↑ David A. Benaron, Katsuyuki Yamamoto, Masatsugu Niwayama, Ling Lin, Toshikazu Shiga, Nobuki Kudo, Makoto Takahashi, Britton Chance, Marco Ferrari, <title>Accurate NIRS measurement of muscle oxygenation by correcting the influence of a subcutaneous fat layer</title>, volume 3194, 1998, pages 166–173, ISSN 0277786X, doi 10.1117/12.301049
- ↑ 80.0 80.1 YN. Bhambhani, Muscle oxygenation trends during dynamic exercise measured by near infrared spectroscopy., Can J Appl Physiol, volume 29, issue 4, pages 504-23, Aug 2004, PMID 15328597
- ↑ R. Belardinelli, TJ. Barstow, J. Porszasz, K. Wasserman, Skeletal muscle oxygenation during constant work rate exercise., Med Sci Sports Exerc, volume 27, issue 4, pages 512-9, Apr 1995, PMID 7791581
- ↑ 82.0 82.1 B. Grassi, V. Quaresima, C. Marconi, M. Ferrari, P. Cerretelli, Blood lactate accumulation and muscle deoxygenation during incremental exercise., J Appl Physiol (1985), volume 87, issue 1, pages 348-55, Jul 1999, PMID 10409594
- ↑ 83.0 83.1 83.2 AC. Snyder, MA. Parmenter, Using near-infrared spectroscopy to determine maximal steady state exercise intensity., J Strength Cond Res, volume 23, issue 6, pages 1833-40, Sep 2009, doi 10.1519/JSC.0b013e3181ad3362, PMID 19675475
- ↑ R. Belardinelli, D. Georgiou, TJ. Barstow, Near infrared spectroscopy and changes in skeletal muscle oxygenation during incremental exercise in chronic heart failure: a comparison with healthy subjects., G Ital Cardiol, volume 25, issue 6, pages 715-24, Jun 1995, PMID 7649420
- ↑ B. Wang, G. Xu, Q. Tian, J. Sun, B. Sun, L. Zhang, Q. Luo, H. Gong, Differences between the Vastus Lateralis and Gastrocnemius Lateralis in the Assessment Ability of Breakpoints of Muscle Oxygenation for Aerobic Capacity Indices During an Incremental Cycling Exercise., J Sports Sci Med, volume 11, issue 4, pages 606-13, 2012, PMID 24150069
- ↑ JA. Davis, R. Rozenek, DM. DeCicco, MT. Carizzi, PH. Pham, Comparison of three methods for detection of the lactate threshold., Clin Physiol Funct Imaging, volume 27, issue 6, pages 381-4, Nov 2007, doi 10.1111/j.1475-097X.2007.00762.x, PMID 17944661
- ↑ T. Reilly, V. Woodbridge, Effects of moderate dietary manipulations on swim performance and on blood lactate-swimming velocity curves., Int J Sports Med, volume 20, issue 2, pages 93-7, Feb 1999, doi 10.1055/s-2007-971099, PMID 10190768
- ↑ 88.0 88.1 T. Yoshida, Effect of dietary modifications on lactate threshold and onset of blood lactate accumulation during incremental exercise., Eur J Appl Physiol Occup Physiol, volume 53, issue 3, pages 200-5, 1984, PMID 6542853
- ↑ N. Maassen, MW. Busse, The relationship between lactic acid and work load: a measure for endurance capacity or an indicator of carbohydrate deficiency?, Eur J Appl Physiol Occup Physiol, volume 58, issue 7, pages 728-37, 1989, PMID 2737193
- ↑ TM. McLellan, GC. Gass, The relationship between the ventilation and lactate thresholds following normal, low and high carbohydrate diets., Eur J Appl Physiol Occup Physiol, volume 58, issue 6, pages 568-76, 1989, PMID 2731528
- ↑ M. Gleeson, AK. Blannin, NP. Walsh, CN. Field, JC. Pritchard, Effect of exercise-induced muscle damage on the blood lactate response to incremental exercise in humans., Eur J Appl Physiol Occup Physiol, volume 77, issue 3, pages 292-5, Feb 1998, doi 10.1007/s004210050336, PMID 9535593
- ↑ RC. Davies, AV. Rowlands, DC. Poole, AM. Jones, RG. Eston, Eccentric exercise-induced muscle damage dissociates the lactate and gas exchange thresholds., J Sports Sci, volume 29, issue 2, pages 181-9, Jan 2011, doi 10.1080/02640414.2010.526626, PMID 21170804
- ↑ CL. de Barros, TT. Mendes, LÁ. Mortimer, HG. Simões, LS. Prado, U. Wisloff, E. Silami-Garcia, Maximal lactate steady state is altered in the heat., Int J Sports Med, volume 32, issue 10, pages 749-53, Oct 2011, doi 10.1055/s-0031-1277191, PMID 21590640
- ↑ T. Meyer, HH. Gabriel, M. Auracher, J. Scharhag, W. Kindermann, Metabolic profile of 4 h cycling in the field with varying amounts of carbohydrate supply., Eur J Appl Physiol, volume 88, issue 4-5, pages 431-7, Jan 2003, doi 10.1007/s00421-002-0712-3, PMID 12527974
- ↑ S. Seiler, What is best practice for training intensity and duration distribution in endurance athletes?, Int J Sports Physiol Perform, volume 5, issue 3, pages 276-91, Sep 2010, PMID 20861519